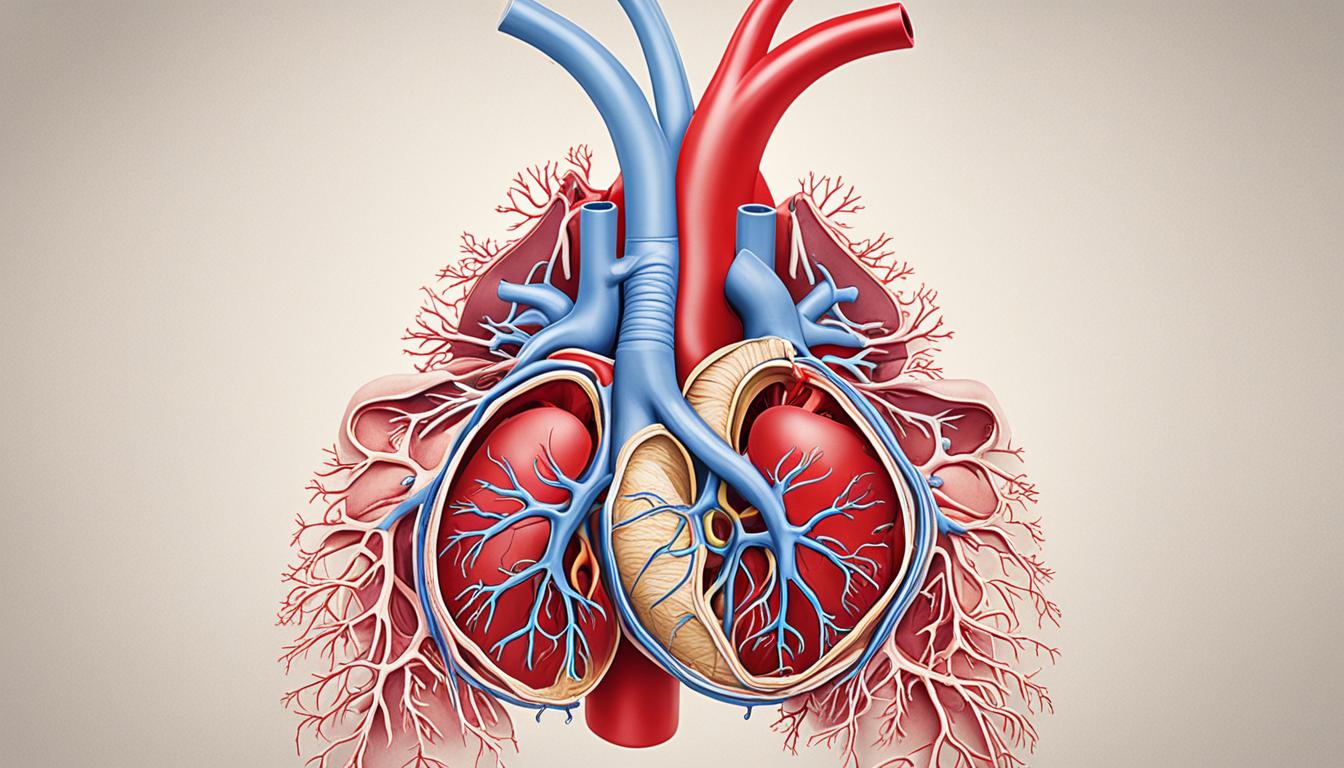
Ventricular septal defects (VSDs) are very common heart issues found at birth or soon after. They happen when a wall in the heart doesn’t close right. This results in a hole between the heart’s lower chambers.
This hole can cause problems. People with VSDs might have a blue skin color, can’t gain weight, breathe quickly, feel tired, or swell. The causes can be due to different health issues during pregnancy. These may include genetic mutations or infections the mother had.
Doctors find VSDs by checking your signs, using special heart images, and maybe looking inside with a thin tube. These tests help figure out how big the hole is and where it is in the heart.
The main fix for big VSDs is surgery. In surgery, the heart’s wall is closed, fixing the hole. Smaller holes might not need surgery because they could close on their own.
Not treating VSDs can cause severe health problems like heart failure or stroke. It’s crucial to watch and maintain these heart issues closely for a better health outcome.
Scientists are studying using stem cells to treat VSDs. This new kind of therapy seems promising. It aims to help the heart grow and work better.
Key Takeaways:
- Ventricular septal defects (VSDs) are the most common congenital cardiac anomaly in children.
- Symptoms of VSDs include cyanosis, poor weight gain, rapid breathing, fatigue, and swelling.
- Causes of VSDs can be developmental abnormalities, chromosomal abnormalities, genetic mutations, or maternal infections or exposures to toxins during pregnancy.
- Diagnosis involves physical examinations, imaging tests, and sometimes cardiac catheterization.
- Surgical repair is the main treatment method for significant VSDs, but smaller defects may close on their own.
- Untreated VSDs can lead to complications such as heart failure, pulmonary hypertension, arrhythmias, and stroke.
- Stem cell therapy shows promise as an innovative treatment option for repairing VSDs.
Types and Classification of Ventricular Septal Defects
Ventricular septal defects (VSDs) are found in different parts of the heart. They have their own unique traits. Knowing about these types helps doctors diagnose and plan the right treatment.
Infundibular (Outlet) VSD
Infundibular VSDs are under the semilunar valves in the outlet septum. They are rare but seen more in Asians. These VSDs connect the right ventricle to the pulmonary artery, causing unusual blood flow.
Perimembranous VSD
Perimembranous VSDs happen on the membranous septum and are the most common. They are near the atrioventricular valves. These defects vary in size and can form a pathway between the right and left ventricles.
Inlet or Atrioventricular Canal VSD
Inlet or Atrioventricular Canal VSDs are below the inlet valves in the right ventricular septum. They are linked to issues in the atrioventricular canal’s growth. This can lead to a lot of blood moving between the heart’s ventricles.
Muscular (Trabecular) VSD
Muscular VSDs are in the heart’s muscular septum. They might be numerous, like a “Swiss cheese.” Often, they are found far from the valves. The size and location can change how blood flows between the heart chambers.
Gerbode Defect
The Gerbode defect is rare and directly connects the left ventricle to the right atrium. This abnormality causes different blood flow patterns. It can lead to serious issues like heart murmurs and heart failure.
Knowing about VSD types helps medical teams choose the best care. They can plan exact treatments. This makes a big difference in how well patients do and their quality of life.
Symptoms, Complications, and Management of Ventricular Septal Defects
Symptoms, Complications, and Management of Ventricular Septal Defects
Ventricular septal defects, or VSDs, cause different symptoms based on their size and severity. Smaller VSDs might not show any symptoms. But, larger ones can result in visible issues and complications.
Typical symptoms of VSDs are:
- Rapid breathing
- Poor weight gain
- Cyanosis (bluish tint to the lips, skin, or nails)
- Fatigue and easy tiring
- Swelling in the legs, feet, or abdomen
If you spot any of these symptoms, it’s crucial to see a doctor. Getting a diagnosis early and taking action can prevent further health problems.
Not fixing VSDs can cause various issues, such as:
- Heart failure due to the strain on the heart.
- High blood pressure in the lungs, noted as pulmonary hypertension.
- Irregular heart rhythms, known as arrhythmias.
- Blood clots that may lead to a stroke in some rare cases.
The approach to managing VSDs involves a team effort. This includes visits to a heart specialist for regular checks. Doctors might also prescribe medicine to deal with symptoms and avoid complications. For significant VSDs, surgery is often the best choice, especially if they’re causing problems.
Small VSDs might heal on their own without surgical help. But the larger ones generally need surgery to prevent issues and ensure a better health outlook in the future.
Management Approaches for Ventricular Septal Defects
| Approach | Description |
|---|---|
| Regular Follow-ups | Monitoring the VSD and assessing its progression over time through regular appointments with a cardiologist. |
| Medication | Prescribing medications to manage symptoms, control blood pressure, or prevent complications associated with VSDs. |
| Surgical Repair | Performing a surgical procedure to close the VSD and restore normal blood flow between the ventricles. |
Conclusion
Ventricular septal defects (VSDs) are a common problem in the heart. They can affect someone’s health and growth. It is key to find VSDs early and treat them right to help patients do well.
Surgical repair is often needed for bigger VSDs. This treatment works well for many. But, some smaller defects can heal themselves without any surgery. Yet, new treatments like stem cell therapy for VSD are being explored thanks to science and tech advances.
Stem cell therapy shows a lot of hope for the future in fixing VSDs. It uses the power of stem cells to heal the heart’s damaged parts. As we learn more and make progress, this could offer a better choice than surgery for some people with VSD.
Thanks to better ways to spot VSDs and many treatment choices, life can be good for those with VSDs. Good care and the progress in medicine bring hope for a better tomorrow for VSD patients.