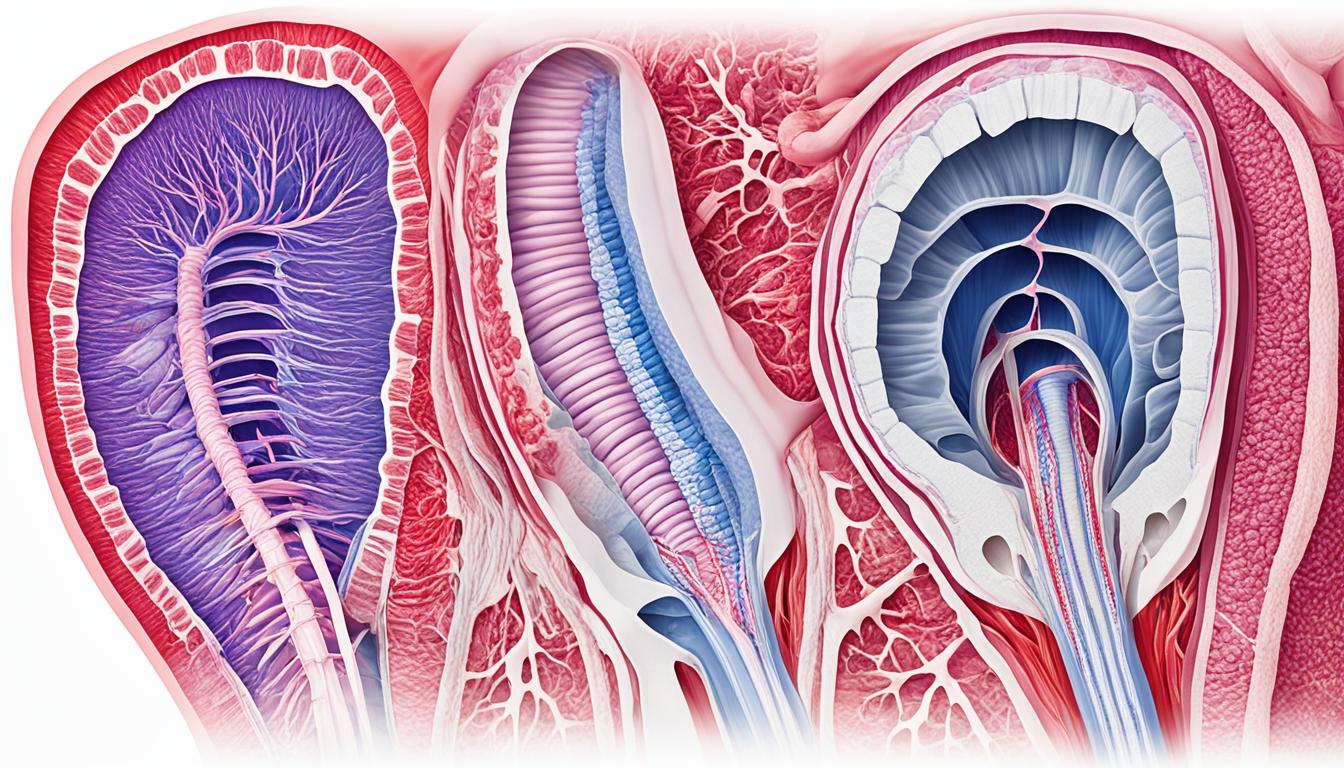
Esophageal varices are found in the lower esophagus. They come from high blood pressure in the portal vein, mostly from liver cirrhosis. If they break, severe bleeding can occur and be life-threatening without quick treatment. Signs of a problem include seeing blood in vomit or bowel movements. Other warning signs are dizziness and fainting. Roughly 30% of those with liver cirrhosis may develop this issue, and it can also hinge on your blood’s ability to clot or certain infections. This urgent situation can cause shock or even take a life. Doctors have ways to handle this, such as reducing blood flow, tying off the affected area, or more extreme steps like a liver transplant. It’s key to start treatment early to better your chances.
Key Takeaways:
- Esophageal varices are abnormalities in the lower part of the esophagus caused by portal hypertension.
- Bleeding is the main symptom of esophageal varices and can be life-threatening.
- Cirrhosis is the primary cause of esophageal varices, with nearly 30% of cirrhotic patients experiencing bleeding.
- Treatment options for esophageal varices include medications, ligation of the varices, portal vein catheterization, and liver transplantation.
- Early diagnosis and treatment are crucial to prevent complications and improve outcomes.
Diagnosing Esophageal Varices and Management Strategies
The diagnosis of varices esophagus usually happens during an endoscopic exam. This exam lets doctors see the veins in your esophagus. People with liver issues, like cirrhosis, need regular checks to catch varices esophagus early.
Once you know you have esophageal varices, it’s all about managing them. The goal is to stop problems and lower the chance of bleeding. Lifestyle changes are the first step. It’s important to avoid very hot or cold foods, and get enough exercise and rest.
Medicines might also be part of managing varices esophagus. These drugs help to lower blood pressure in the portal vein, which can reduce bleeding risk. The exact medicine you’d get depends on your health and the severity of your varices.
For severe cases, surgery could be needed. There are two main types: ligation and TIPS. Ligation stops varices from bleeding by tying them up. TIPS surgery creates a new path for blood to avoid the varices.
Prevention and Regular Follow-Up
Keeping up with your health through regular visits is key. If you have esophageal varices, seeing your doctor often is a must. They’ll check on your condition and adjust your care plan as needed.
In the end, spotting diagnosing esophageal varices is about seeing the veins directly. Managing them aims to prevent problems and lower the chance of bleeding. This involves lifestyle changes, possibly medicine, and sometimes surgery. Staying in touch with your doctor is very important for long-term care.
Stem Cell Therapy for Esophageal Varices
Stem cell therapy is a new way to treat esophageal varices. This condition affects the blood vessels in the esophagus. It uses stem cells that can change into different cell types. This helps promote healing and growth of tissues.
This therapy can make the blood vessels in the esophagus work and look better. It tackles the main problems, which lowers the chance of bleeding and other issues. Patients with esophageal varices can find hope in this treatment.
Research on this therapy is still starting, but the first studies are promising. Yet, more studies are needed to guarantee its safety and success. People thinking about this treatment should talk to their doctors. Joining clinical trials might give them the chance to try this new method.
Stem cell therapy is changing the game in treating esophageal varices. It offers a way to get better results and improve life quality. With the help of experts and continuous research, the future looks hopeful for those with this condition.