Uterine prolapse happens when the pelvic floor weakens. This lets the uterus drop down into the vagina or even stick out. It’s more likely to occur in women after childbirth, especially if they’ve had several or delivered vaginally. Being older, overweight, coughing a lot, or having a family history also increases the risk.
The signs of uterine prolapse can vary. You might feel pelvic heaviness or see a bulge in the vagina. Backaches, peeing a little when you don’t want to, and trouble pooping are also common.
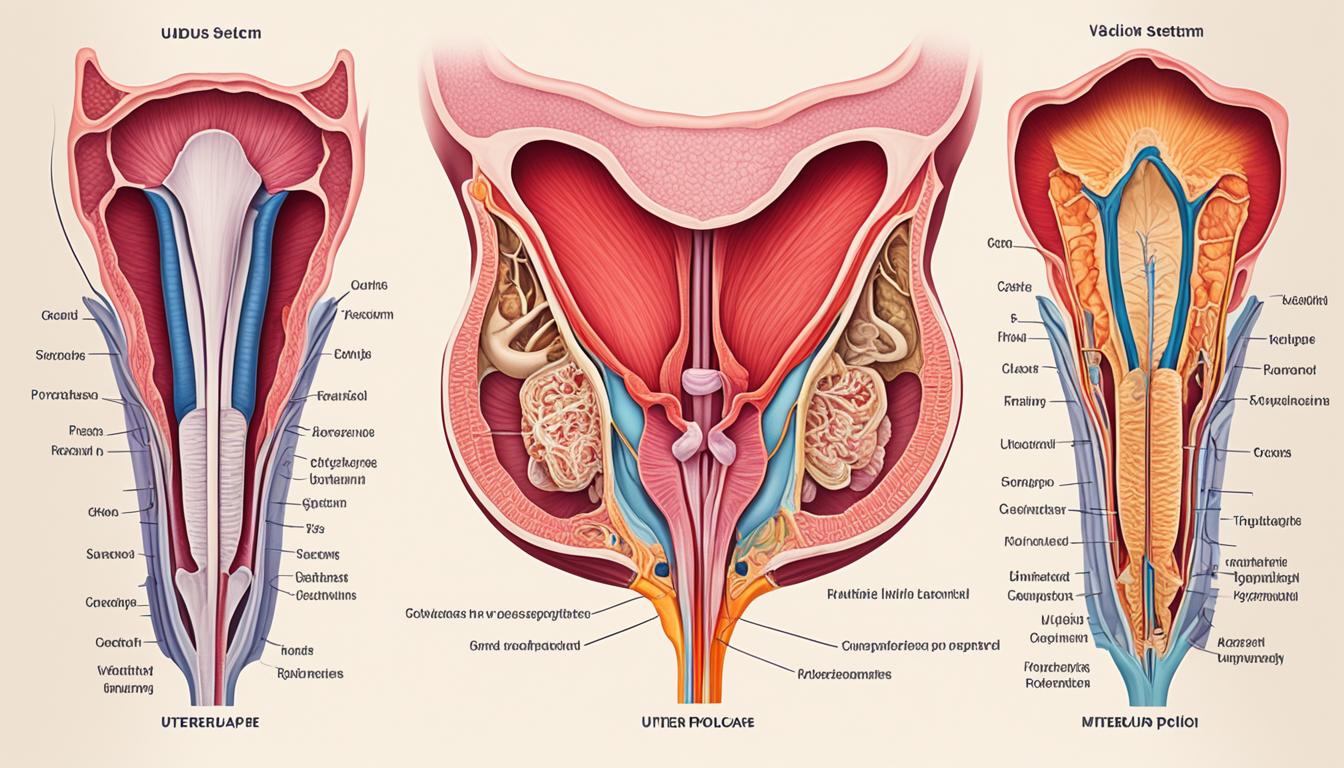
Your doctor will check you physically to diagnose this. They might also use tests like ultrasound or MRI.
To manage uterine prolapse, start with lifestyle changes and special exercises. A pessary, a device placed in the vagina, is another option. For more serious cases, surgery could be needed.
Key Takeaways:
- Uterine prolapse affects women when the uterus falls into the vagina due to muscle and ligament weakness.
- Common risk factors are giving birth, getting older, being overweight, coughing a lot, and having family history.
- Symptoms may include a heavy feeling in the pelvis, back pain, leaks when urinating, difficulty with bowel movements, and a visible bulge.
- Your doctor will likely diagnose this through a physical test and possibly with ultrasound or MRI.
- Treatments vary from lifestyle changes and exercises to a pessary or surgery in more severe cases.
Causes and Risk Factors of Uterine Prolapse
Uterine prolapse happens when the uterus falls into the vagina. It can occur due to several reasons. Tearing the pelvic floor during childbirth is a main reason. This is more likely with intense, long labors. Not resting enough after giving birth and overworking can also weaken the uterus’s support.
Issues in the uterus from birth and post-delivery bowel problems can be blamed too. Such birth issues can make you more likely to have prolapse. Bowel issues after birth may also strain the pelvic muscles, adding to the problem.
Several things raise the odds of uterine prolapse. These include twin or multiple pregnancies, being older, or having many children. Hard labors, uterine surgeries, and issues with the placenta can also increase the risk. Past surgeries on the uterus also make you more at risk.
Knowing these causes and risks is key to preventing and treating uterine prolapse. It helps doctors create good plans to help. And it guides ways to lower the risk of prolapse.
| Risk Factors | Causes |
|---|---|
| Pregnancy with twins or multiples | Trauma to pelvic floor during childbirth |
| Advanced age | Working too hard after delivery |
| Multiple pregnancies | Birth defects in the uterus |
| Difficult delivery | Postpartum bowel disorders |
| Prolonged uterine ligation | |
| Placental abnormalities | |
| Previous uterine surgeries |
Symptoms and Diagnosis of Uterine Prolapse
Uterine prolapse symptoms change based on how serious it is. Painful feeling or pressure in the pelvis, backache, and trouble controlling pee are common. So are issues with pooping and a noticeable bulge in the vaginal area. These signs can really change a woman’s life for the worse and should be taken seriously.
Doctors check for uterine prolapse with a physical exam first. This often uses a speculum to look inside. Ultrasounds or MRIs might also be used to see the extent of the prolapse and eliminate other issues. Catching it early helps manage uterine prolapse better.
Treatment and Management of Uterine Prolapse
The way we treat uterine prolapse depends on how bad it is and how much it affects a woman’s life. For small issues, we might not need surgery. Changing your lifestyle can make a big difference. This includes staying at a healthy weight, not lifting heavy things, and doing exercises to strengthen your pelvic floor. These changes can lower symptoms and stop the condition from getting worse.
Kegel exercises are great for this. They make your pelvic floor muscles stronger and support your uterus better. Kegels just involve squeezing and letting go of certain muscles. Doing these exercises often can really help with symptoms and stop the prolapse from getting worse.
Some women might find a pessary helpful. This is a small tool that goes into the vagina to help hold up the uterus. There are many types of pessaries. The right one depends on what’s most comfortable for you.
If the problem is bad and other treatments haven’t worked, surgery could be an option. There are a few different surgeries available. The choice of surgery depends on how severe the prolapse is and your health goals. Talking with a doctor is important to figure out the best plan. After treatment, it’s key to have regular check-ups and look after yourself.
It’s also important to try and prevent uterine prolapse. Keeping a healthy weight and not pushing your body too hard helps. If you have a condition that makes you cough a lot or get constipated, getting treatment for that is also important. This all helps lower your chances of getting prolapse again.