Blood in the urine, known as
hematuria
, is a frequent symptom in many diseases. It can signal a serious health issue. There are two main types:
gross hematuria
(visible blood in urine) and
microscopic hematuria
(blood cells in urine found only with a microscope).
Lots of things can cause hematuria. These include urinary tract infections, kidney stones, or bladder infections. It can also show up in kidney disease, bladder cancer, or urinary tract cancer.
Doctors work hard to find the cause of hematuria. They may do a physical check-up and tests, like urine, imaging (ultrasound or CT), or sometimes a cystoscopy or biopsy.
What you need for hematuria treatment depends on the cause. Sometimes, nothing specific is needed, and it goes away by itself. But if it’s serious, you’ll get the right treatment. Stem cell therapy is also an option in some cases.
If you see blood in your urine, don’t wait. Go see a doctor right away. This is key to finding out what’s wrong and how to treat it.
Key Takeaways:
- Seeing blood in your urine might mean you have a disease.
- Gross hematuria means you can see the blood, while microscopic hematuria needs a microscope to see it.
- It can be from infections, kidney stones, trauma, or big issues like cancer.
- Finding out the cause means many different tests.
- How they treat it changes based on what’s causing the blood.
Types of Myelodysplastic Syndromes (MDS) and Symptoms
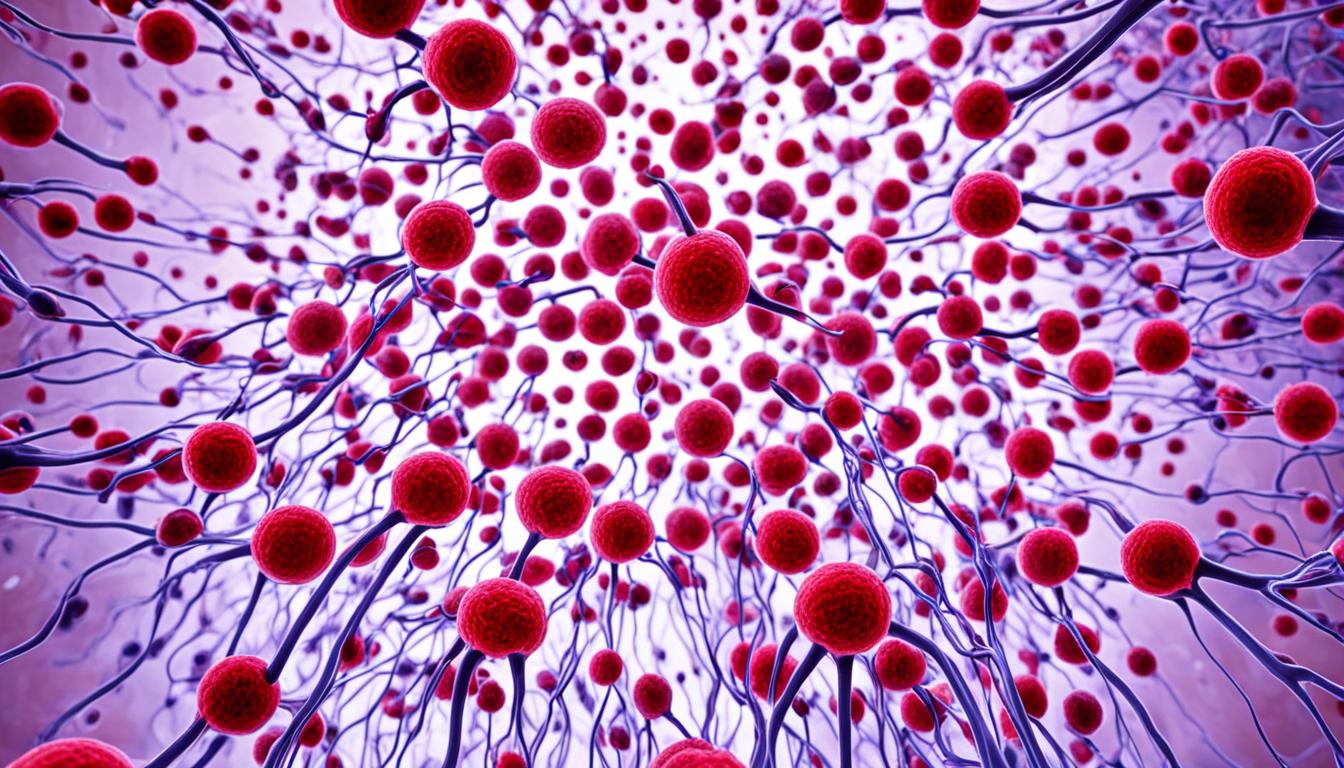
Myelodysplastic syndromes (MDS) are a group of related conditions. They impact the body’s ability to produce healthy blood cells in the bone marrow. MDS comes in various types, each presenting unique characteristics and symptoms.
MDS with Single Lineage Dysplasia
MDS with single lineage dysplasia means certain blood cell lines don’t develop normally. It shows up as issues like refractory anemia, thrombocytopenia, and neutropenia. To diagnose it, doctors use blood tests, bone marrow biopsy, and examine blood cells closely.
MDS with Ring Sideroblasts
In MDS with ring sideroblasts, red blood cell precursors hold iron-filled mitochondria. This often leads to symptoms such as anemia, tiredness, and an enlarged spleen. Doctors use tests on blood and bone marrow to spot these ring sideroblasts for a diagnosis.
MDS with Multilinear Dysplasia
MDS with multilinear dysplasia disrupts the development of several blood cell lines. It causes problems in red blood cells, white cells, and platelets. The symptoms vary based on which cell type is affected. Doctors confirm the diagnosis with blood tests, bone marrow biopsy, and special cell analysis.
MDS Unclassified
MDS unclassified doesn’t neatly fall into a single subtype. But it shows dysplastic changes in the blood cells. Its symptoms and diagnostic procedures are often similar to other MDS types.
MDS Associated with Isolated del(5q)
In MDS tied to an isolated del(5q), a specific part of chromosome 5 is missing. This affects red blood cell production the most. Anemia and physical changes are common symptoms. Detecting it needs genetic tests and bone marrow examination.
MDS with Excess Blasts-1 and MDS with Excess Blasts-2
MDS with excess blasts-1 and -2 refer to more severe cases. They have a lot of abnormal blast cells in the bone marrow. This can cause anemia, infections, or bleeding. Doctors diagnose it by checking the marrow for blast cells.
Remember, MDS is diagnosed and treated by healthcare professionals. Treatment options vary, from supportive care to stem cell transplants. The choice depends on the MDS subtype and the patient’s prognosis.
Conclusion
Myelodysplastic syndromes (MDS) are a form of blood cancer. They impact the formation of healthy blood cells in the bone marrow. Being diagnosed with MDS includes several tests like blood tests and genetic testing. How well someone does with MDS is complex. It depends on the MDS type, its stage, and the person’s health.
Treatments for MDS help with symptoms and slow down the disease. They can make life better. Supportive care, blood transfusions, and certain medications are common treatments. For some, a stem cell transplant can provide a cure.
A stem cell transplant swaps out sick bone marrow with healthy stem cells. It can be a big help but not everyone can have it. The decision is based on age, health, and certain gene changes.
In recent times, things have gotten better for people with MDS. Understanding MDS more and new treatments have helped. It’s crucial for those with MDS to get the right advice. Talk with your healthcare team about what’s best for you.