Tinea corporis is a common fungal infection. It affects the skin, hair, and nails. This disease comes from certain fungi. You can get it by touching infected people, animals, or items. The symptoms are itchy skin, red and scaly patches in a ring, and small bumps with pus.
A doctor can diagnose tinea corporis by looking under a microscope or growing the fungus in a lab. Treatments include putting antifungal cream on the skin or taking antifungal pills. There’s also talk about using stem cell therapy to treat it.
Key Takeaways:
- Tinea corporis is a contagious fungal skin infection caused by dermatophyte fungi
- Common symptoms include itchiness, red and scaly patches with a ring-like appearance, and small papules and pustules at the periphery
- Diagnosis can be confirmed through direct microscopy or fungal culture
- Tinea corporis can be treated with topical antifungal creams or oral antifungal medications
- Stem cell therapy is an emerging treatment approach for tinea corporis
Causes and Transmission of Tinea Corporis
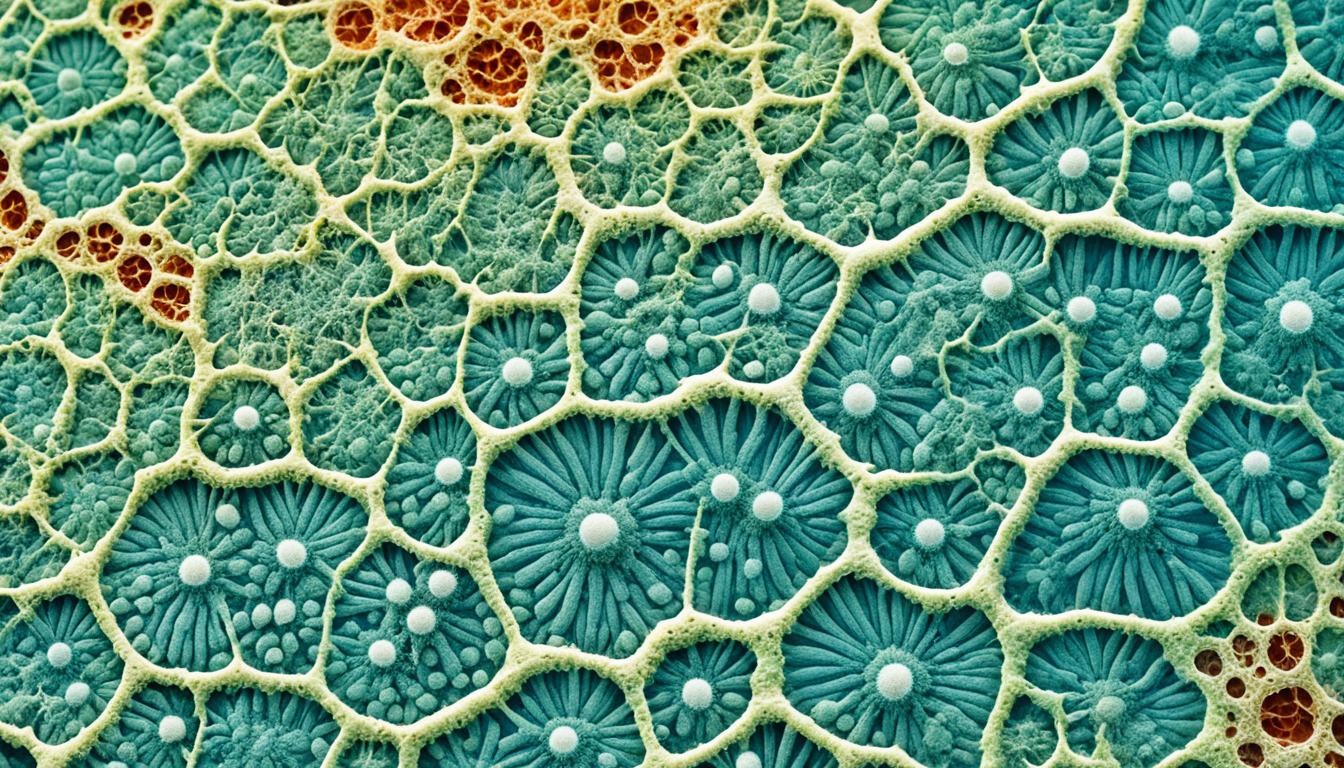
Tinea corporis is a skin infection caused by a type of fungi. These fungi target keratinized tissues, like the skin. The fungi mainly belong to the genera Trichophyton, Microsporum, and Epidermophyton.
This infection spreads through direct contact. It can move from an infected person or animal to another. Such contact includes touching infected skin or sharing items like towels.
Also, the infection can spread within the same person. This can happen if you scratch the infected area and then touch healthy skin.
Several factors make you more likely to get tinea corporis. These include lots of skin contact, tight clothing, and humid weather. These help the fungi grow and spread.
Dermatophyte species and their prevalence
Different species of dermatophytes can cause tinea corporis. But, the most common ones are Trichophyton rubrum, Trichophyton mentagrophytes, and Microsporum canis. They are widely found in cases of this infection.
| Dermatophyte Species | Prevalence |
|---|---|
| Trichophyton rubrum | Most prevalent worldwide |
| Trichophyton mentagrophytes | Common cause of athlete’s foot and other dermatophyte infections |
| Microsporum canis | Major cause of tinea capitis (scalp ringworm) |
To stop the infection, knowing how it spreads and proper diagnosis is important.
Symptoms, Diagnosis, and Complications of Tinea Corporis
Ringworm, also called tinea corporis, has noticeable signs. It starts with itchiness and a red, scaly patch on the skin. This patch often has a clear outer edge and can develop small bumps. If not treated, it becomes larger and looks like a ring on the skin.
Doctors can find out if you have tinea corporis by looking at a skin sample under a microscope. This helps them see the specific fungus causing the infection. Another method is fungal culture, where the skin sample is grown in a lab to figure out the fungus type.
Sometimes, tinea corporis is hard to diagnose, especially if steroid creams have been used. These creams can change how the infection looks. This makes it harder to tell it apart from similar skin issues. Such a changed pattern is called “tinea incognito.”
Treating tinea corporis with the wrong medicines because of a misdiagnosis can cause the infection to last longer. This might also make it spread to other parts of the body. Other skin problems, like psoriasis or eczema, can be mistaken for ringworm, causing delays.
Complications of Tinea Corporis:
- Misdiagnosis with other skin conditions
- Delayed or inappropriate treatment
- Potential spread of infection
| Symptoms | Diagnosis | Complications |
|---|---|---|
| Itchiness | Direct microscopy | Misdiagnosis |
| Red, scaly patch | Fungal culture | Delayed treatment |
| Papules and pustules | Spread of infection | |
| Ring-like appearance |
Treatment and Prevention of Tinea Corporis
Tinea corporis is a type of skin infection caused by a fungus. It can be treated well with antifungal medicines. The treatment used varies. It depends on the size and spread of the infection. It also considers how well the person responds to the first treatment. Plus, the chance of the infection coming back matters.
To treat small infections, use creams. These creams have imidazole, allylamine, tolnaftate, or cicloprox. Put the cream on the infected area two times a day. Keep using it for two to four weeks. The creams stop the fungus. This way, the infection goes away.
If the infection is big or the cream doesn’t work, you might need pills. Doctors can give you itraconazole, terbinafine, or fluconazole. You take these pills. They kill the infection from the inside out.
Preventing the infection is as important as treating it. Never share towels or clothes. This can spread the infection to others. Also, keep the skin dry. Fungi like warm, wet places. Doing these things can prevent the infection from coming back.