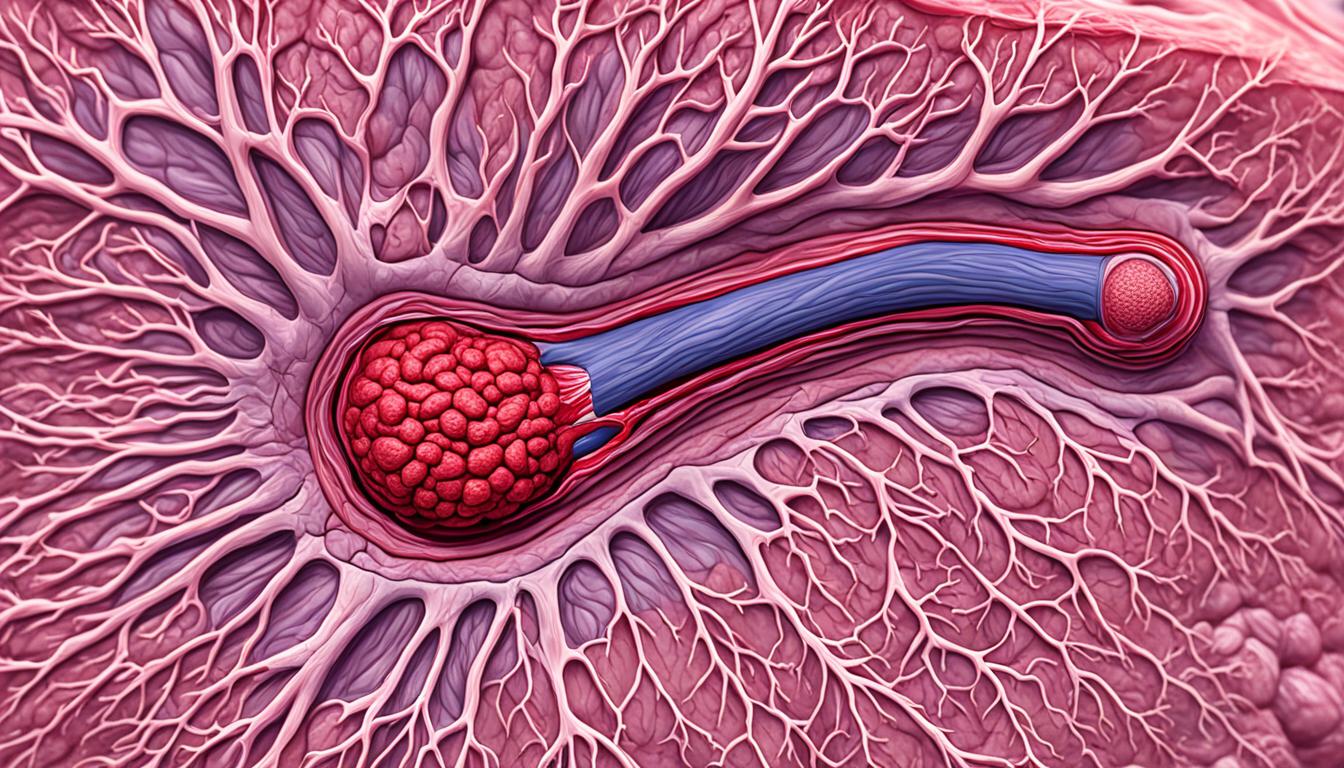
Thrombophlebitis is when a vein gets inflamed due to a blood clot. It can happen in veins close to the skin’s surface or deep within muscles. Causes include issues like catheter-related clotting and events where blood clots move in the veins. People with cancer, head injuries, or those who have spent a long time in the hospital are more at risk. For patients who had a stem cell transplant, about 3.7% might get a blood clot in a vein.
The main aim in treating thrombophlebitis is to avoid dangerous complications and keep the catheter open. While doctors use some common ways to treat it, they’re also looking at how stem cell therapy might help. This shows promise as a new method to tackle thrombophlebitis.
Key Takeaways:
- Thrombophlebitis happens when a vein gets inflamed and a clot forms.
- It can affect veins near the skin or deeper in the body, which is risky.
- Things like catheter issues and certain events can lead to thrombophlebitis.
- Having dealt with a head injury, stayed in the hospital long, or used central venous catheters can raise the risk.
- Stem cell treatment is a new, promising area for dealing with thrombophlebitis.
Phlebitis: Symptoms, Causes, and Diagnosis
Phlebitis is the swelling of veins, falling into two types: superficial and deep. Superficial phlebitis is often from outside sources like IVs or harsh fluids. It goes away by itself once the cause is gone. But deep phlebitis, termed thrombophlebitis, comes with a blood clot.
The signs of phlebitis are pain, swelling, redness, and warmth near the vein. With deep phlebitis, there’s a risk of serious issues, like a blood clot moving to the lungs. Doctors look at symptoms and do tests like ultrasound to diagnose it.
Knowing phlebitis symptoms is key for quick care. Getting medical help at the first sign is vital. Quick treatment stops it from getting worse and causing big problems.
Causes of Phlebitis
Causes differ for superficial and deep phlebitis. Superficial cases often come from vein injuries by IVs or reaction to certain drugs. But, deep phlebitis links with blood clots. These clots can stop blood flow and cause swelling and pain.
Diagnosis of Phlebitis
Diagnosing phlebitis means looking at symptoms and doing tests. The doctor checks for redness and warmth by the vein. They also consider the patient’s history. Tests like ultrasound and CT scans are used to see the veins and find blood clots.
| Signs of Phlebitis | Causes of Phlebitis | Diagnosis of Phlebitis |
|---|---|---|
| Pain | External trauma to the vein | Clinical evaluation |
| Swelling | Intravenous catheterization | Medical history assessment |
| Redness | Irritation from medications or infusions | Imaging tests (ultrasound, CT scan) |
| Warmth | Blood clots in the vein (thrombophlebitis) |
Complications and Treatment of Phlebitis
Superficial phlebitis isn’t usually serious but can lead to infection if not treated. Deep phlebitis, on the other hand, is riskier. It can cause pulmonary embolism, which leads to breathing problems and can be fatal.
Treating phlebitis means dealing with its root cause. You might get anti-inflammatory drugs or antibiotics if there’s an infection. For deep vein thrombosis, you’ll need a more complex plan. This could include medicines to stop blood clots from getting worse. Or treatments like breaking up clots or putting a filter in a major vein.
To stop phlebitis, avoid things like not moving much, smoking, and some drugs. A healthy life with exercise and good food is also key to lower your phlebitis risk.
Complications of Phlebitis:
Deep phlebitis, especially, can cause serious problems. It might lead to blood clots that can be dangerous. Or it could cause a pulmonary embolism, which is a blood clot in your lungs. This can make it hard to breathe and be life-threatening.
Treating phlebitis early is important. It helps prevent these scary issues from happening or getting worse.
Treatment Options for Phlebitis:
How phlebitis is treated depends on how serious it is and where it is. Your doctor might suggest:
- NSAIDs to ease swelling and pain
- Using warm things to feel better and help blood move
- Raising the hurt leg to lessen swelling
- Wearing special socks or wraps to support your leg and stop bad blood flow
- Getting rid of something that’s bothering your vein or an infected tube
- Taking antibiotics if there’s an infection
- Drugs to keep blood clots from forming
- Having surgery to pull out a clot or put in a filter in a big vein
It’s crucial to see a doctor for the right diagnosis and treatment plan for phlebitis.
| Table: Comparison of Superficial Phlebitis and Deep Phlebitis | |
|---|---|
| Superficial Phlebitis | Deep Phlebitis |
| Occurs near the surface of the skin | Affects deep veins within muscles |
| Usually caused by external factors such as IV catheterization or infusion of irritating substances | Often associated with the presence of a blood clot in the vein (thrombophlebitis) |
| Resolves spontaneously with discontinuation of therapy | Requires more complex treatment to prevent complications |
| Pain, redness, swelling, and warmth along the affected vein | Risk of complications such as pulmonary embolism |
Conclusion
Thrombophlebitis is when veins swell and form blood clots. It can affect both deep and surface veins. This condition could lead to serious issues like pulmonary embolism. So, spotting it early and getting treatment is key to avoid complications.
Experts are looking into using stem cells to treat this problem. Stem cells can actually help fix damaged tissues. This makes them an exciting option for thrombophlebitis care. There are lots of studies going on to see how well and safely this treatment works.
It’s important to know how to prevent thrombophlebitis. You can lower your risk by not sitting still for too long, avoiding smoking, and watching what medicines you take. A good diet and regular exercise also help keep your veins healthy and may stop thrombophlebitis from happening.
If you think you might have this condition, don’t wait to get help. A doctor can check you out and figure out the best way to treat it. They might need to do tests to be sure. Getting the right help early can mean a smoother recovery and less chance of complications.