Tay-Sachs disease is a rare genetic disorder. It impacts the nervous system. This disorder means the body lacks an enzyme called hexosaminidase. Without this enzyme, GM2 gangliosides build up in the brain and spinal cord.
The buildup causes a slow loss of nerve cell function. This leads to severe health and mental challenges. Sadly, there isn’t a way to stop or reverse these effects yet.
Key Takeaways:
- Tay-Sachs disease is a genetic disorder that causes neurodegeneration.
- It is caused by a deficiency of the enzyme hexosaminidase, leading to the accumulation of GM2 gangliosides.
- The disease primarily manifests in infancy, with symptoms including developmental delays, muscle weakness, seizures, and cherry-red spots in the retina.
- Diagnosis involves clinical evaluation, blood tests, genetic testing, and eye exams.
- Currently, there is no cure for Tay-Sachs disease, but supportive treatments and potential future therapies, such as gene therapy and stem cell transplantation, are being explored.
Etiology and Pathophysiology of Tay-Sachs Disease
Tay-Sachs disease is a severe genetic disorder that targets the neurons. It causes a gradual loss of neurological functions. The root cause is in the HEXA gene, which makes the Hex A enzyme.
When there are mutations in this gene, Hex A activity drops or stops. This makes it hard for the body to break down GM2 gangliosides. These then build up in the neurons.
GM2 ganglioside buildup starts early in life and continues. We know this affects how cells work, but we’re still learning the full story. Some think it messes with how cells transport and deal with waste, but that’s not yet confirmed.
As cells fail to work normally, the brain starts to lose function. This leads to the symptoms we see in Tay-Sachs disease over time.
Impaired Lysosomal Function in Tay-Sachs Disease
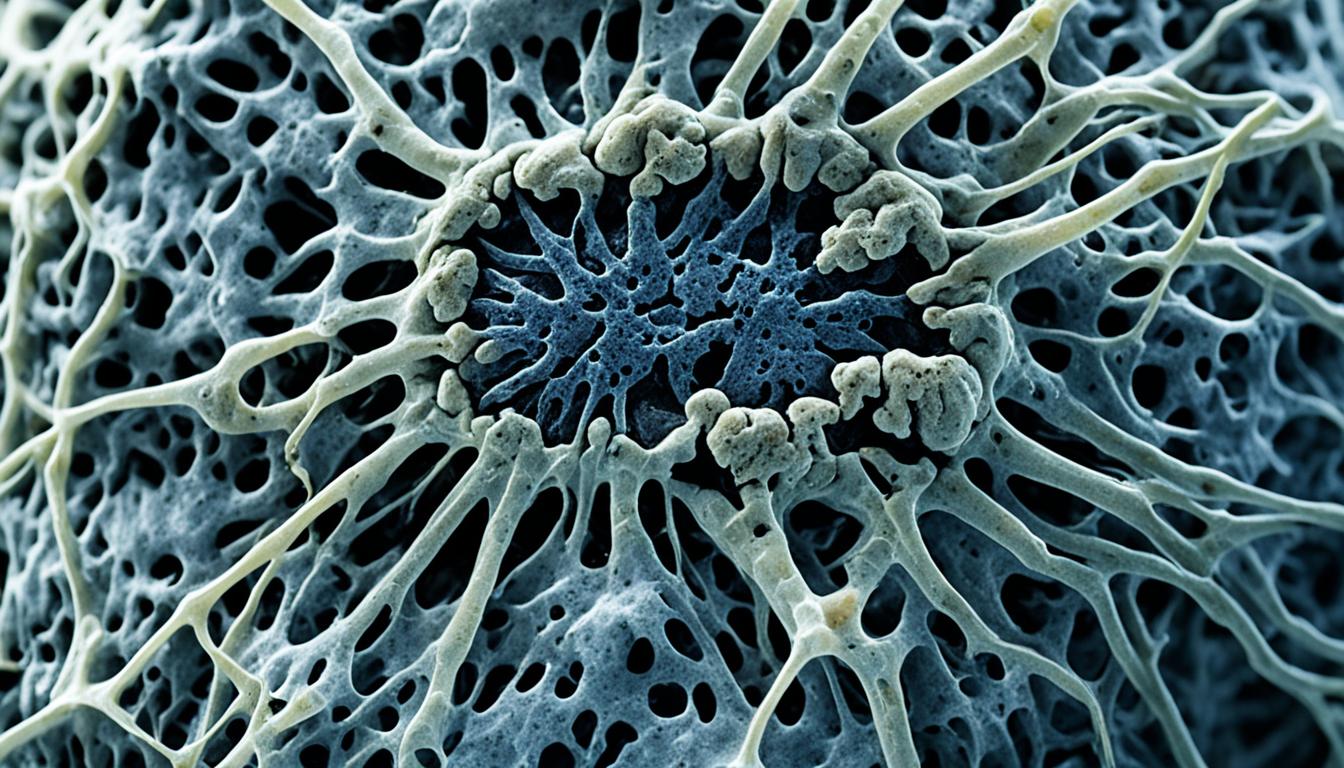
Lysosomal issues are at the heart of Tay-Sachs. Lysosomes help break down cell waste and when they can’t degrade GM2, it accumulates.
This trouble in lysosomes is linked to HEXA gene problems. Without Hex A, lysosomes can’t break down GM2 like they should. So, GM2 builds up.
This image shows how HEXA gene issues, GM2 buildup, and Tay-Sachs connect. It gives us a clear idea of the disease’s development.
By learning more about Tay-Sachs, experts are getting closer to new treatments. Understanding the disease helps find ways to stop its effects.
Diagnosis and Clinical Presentation of Tay-Sachs Disease
Diagnosing Tay-Sachs disease is hard because its signs are subtle. Its markers in tests are also unclear. But, spotting it early is key for the right care. It also helps in guiding the parents well.
The signs of Tay-Sachs change by when they start. In babies, they usually show up between 3 to 6 months. You might see developmental delays, muscle weakness, an exaggerated startle response, cherry-red spots in the retina, seizures, and loss of motor skills.
By age 2, kids might have macrocephaly (an unusually large head). They might also show decerebrate posturing, which is odd body movement. In older children, signs could start in early childhood. This might include incoordination, muscle weakness, ataxia (a lack of muscle coordination), and intellectual disability.
The adult kind of Tay-Sachs is rare. It shows up with fewer signs, like muscle weakness, dysarthria (trouble speaking), and psychiatric symptoms.
To diagnose Tay-Sachs, doctors use a mix of exams and tests. They look at symptoms, check hexosaminidase levels in blood, do genetic tests, and an eye exam. The goal is to spot the disease by these signs and tests. This helps avoid misdiagnosing it with similar issues.
Detailed Clinical Presentation of Tay-Sachs Disease:
- Infantile Form:
- Onset: 3 to 6 months of age
- Developmental delays
- Muscle weakness
- Exaggerated startle response
- Cherry-red spots in the retina
- Seizures
- Loss of motor skills
- Macrocephaly (an abnormally large head)
- Decerebrate posturing (abnormal body posturing)
- Juvenile Form:
- Onset: Early childhood
- Incoordination
- Muscle weakness
- Ataxia (lack of coordinated muscle movement)
- Intellectual disability
- Adult Form:
- Rare
- Muscle weakness
- Dysarthria (difficulty speaking)
- Psychiatric symptoms
Next, we’ll look into possible treatments and where the Tay-Sachs research might go.
Potential Treatments and Future Directions for Tay-Sachs Disease
There’s no cure for Tay-Sachs disease yet, but researchers are working hard. They aim to find ways to make life better for those with the disease. The main focus is on lessening symptoms and giving care that supports a better life.
People with Tay-Sachs might get help with seizures or be given extra care for their breathing needs. Therapy, like physical and occupational therapy, is also important. This kind of therapy helps keep the body moving and working well. Speech therapy can also improve how people swallow when they have difficulty.
For the future, scientists are looking into some exciting new treatments. For example, they want to try replacing the missing enzyme. This may help lessen harmful substances in the body. There’s also work being done on gene therapy. This involves adding working genes to the body to make the missing enzyme. And, stem cell treatments could replace unhealthy cells with new, working ones.
These new treatments are at the start of their journey and need a lot more work before they’re ready. But, there’s a lot of hope. Medical research is always moving forward. This means there could be new, better treatments, and even a cure, for Tay-Sachs disease in the future.