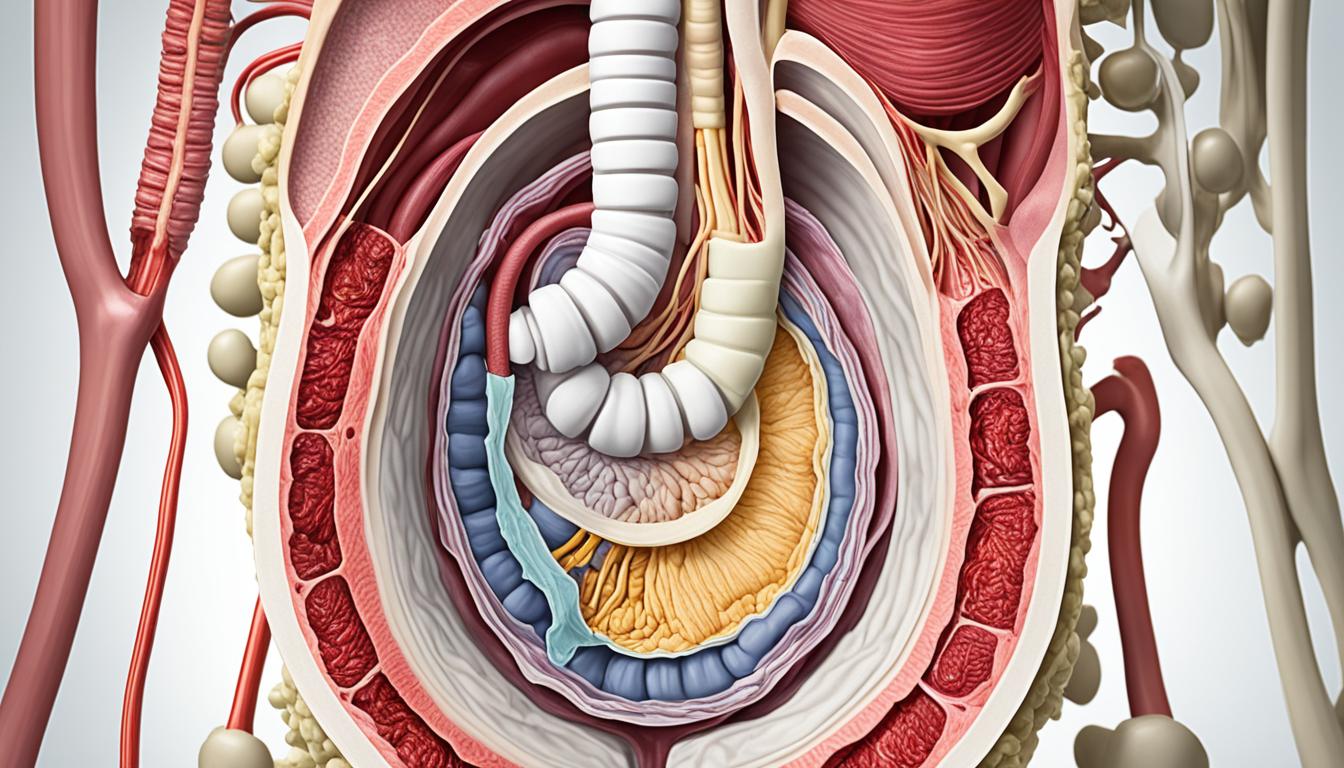
Pelvic floor dysfunction happens when the muscles, ligaments, and tissues get weak or tight. This can lead to symptoms like pain and trouble with bladder and bowel function. Small bowel prolapse, or enterocele, occurs when the small intestine drops and pushes into the vagina. This causes a bulge and can lead to pelvic pain, pressure, and issues with using the bathroom or having sex.
Risk factors for small bowel prolapse include your age, health conditions, pregnancy, and collagen disorders. Treatment includes changing your diet, using laxatives, taking pain medication, and doing exercises to strengthen your pelvic floor. Some people might need surgery to fix the problem. Stem cell therapy is also being explored and seems promising based on animal studies.
Key Takeaways:
- Small bowel prolapse, or enterocele, is a type of pelvic organ prolapse where the small intestine descends into the vagina, causing symptoms such as pelvic pain, pressure, and urinary and bowel dysfunction.
- Risk factors for small bowel prolapse include age, systemic diseases, chronic health issues, pregnancy, trauma during delivery, and collagen disorders.
- Treatment options for small bowel prolapse include dietary changes, medication, pelvic floor rehabilitation, pessary devices, and surgery.
- Stem cell therapy is being researched as a potential treatment option for pelvic floor dysfunction, showing promise in animal studies.
- If you experience symptoms of pelvic floor dysfunction, it is important to consult a healthcare provider for diagnosis and appropriate treatment.
Types of Pelvic Floor Dysfunction
Pelvic floor dysfunction is a group of ailments that harm the muscles, ligaments, and nerves of the pelvic floor. It’s vital to know the different types to treat the symptoms correctly. The common types include:
Obstructed Defecation
It’s hard to pass stool in obstructed defecation due to a blockage issue. This can make you feel like you didn’t finish, need to push a lot, and feel something stuck in your rectum.
Rectocele
Rectal tissue can bulge into the vaginal wall in rectocele. It might be hard to pass stool, feel pressure in the pelvis, or have pain during sex.
Pelvic Organ Prolapse
Pelvic organ prolapse is when the bladder, rectum, or uterus drop down because the pelvic floor is weak or damaged. Signs include a vagina bulge, issues urinating or defecating, and pelvic pain.
Paradoxical Puborectalis Contraction
This issue is when the puborectalis muscle tightens instead of relaxing during a bowel movement. It makes stool hard to pass, feel like you’re not done, and often feels like you’re constipated.
Levator Ani Syndrome
Levator ani syndrome means the pelvic floor muscles have too much tension. It can lead to deep pelvic pain, aching, and pressure in the rectal or vaginal area.
Coccygodynia
Coccygodynia causes ongoing tailbone pain. It might come from a fall or injury to the coccyx. The pain is felt when sitting, standing, or if there’s pressure on the area.
Proctalgia Fugax
In proctalgia fugax, you get sudden, strong rectal pain that doesn’t last. This causes sharp, cramp-like feelings that surprise you. Thankfully, the pain usually goes away on its own.
Pudendal Neuralgia
When the pudendal nerve has problems, it’s called pudendal neuralgia. It can lead to constant pelvic pain, and numbness or tingling in the groin, buttocks, or inner thighs.
Urethrocele
Urethrocele is when the urethra pushes into the vaginal wall. It might lead to leaking urine, urinary infections, and painful urination.
Enterocele
Enterocele happens when the small intestine pushes into the vaginal wall. This causes pelvic pain, pressure, or a full feeling low in the pelvis.
Cystocele
A cystocele is when the bladder bulges into the vagina. It might cause you to leak urine, have urinary infections often, or feel discomfort in the pelvis.
Uterine Prolapse
Uterine prolapse is the uterus dropping into the vagina. Signs include a bulge at the vaginal opening, urinary and bowel issues, and pelvic pain.
These pelvic floor issues can change how you live, causing physical pain and emotional stress. It’s crucial to see a specialist for proper care and relief.
Stem Cell Therapy for Small Bowel Prolapse
Experts are looking to stem cell treatments for pelvic floor issues like small bowel prolapse. They’ve found that in animals, stem cells which make elastin and collagen can fix the structures of the pelvic floor. This helps ease symptoms like leaking urine under stress. New stem cells have also been created to boost elastin in the pelvic floor area.
More studies are needed to see how well these therapies work in people. But, they are very promising for treating problems with the pelvic floor. So, if you have symptoms like painful bowel movements or trouble with urinating, it’s important to see a doctor. They can find out what’s wrong and recommend the best treatment.
Doctors can diagnose pelvic floor issues with a detailed exam. Treatment might involve changing your diet, taking medicines, or doing special exercises. In more serious cases, surgery could be an option. It’s key to get help from a healthcare expert to feel better and manage these symptoms.