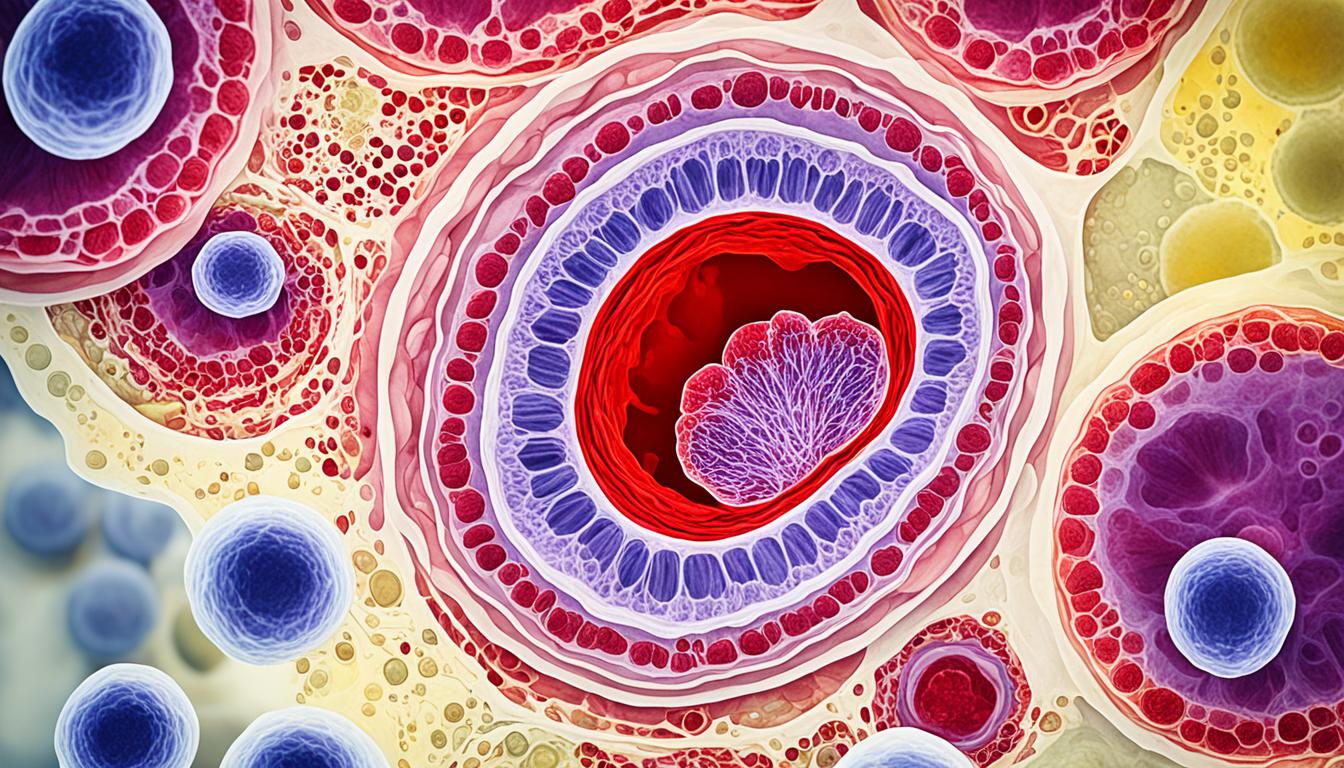
Pseudomembranous colitis is a kind of inflammatory bowel disease. It happens to some people after they take antibiotics. This disease is due to too much of a bacteria known as Clostridium difficile (C.difficile). When these bacteria let out strong toxins, they cause bad irritation and swelling in the intestines. This leads to the creation of white pseudomembranes. Those with this condition might feel fever, stomach pain, and frequent diarrhea. Sometimes, the stool might have blood or mucus. In severe situations, it can lead to very dangerous problems like a broken colon or infections inside the belly. People over 65, those with weak immunity, some health problems, or a past of gut surgery, or lots of hospital stays, are at a bigger risk. Getting diagnosed and treated early is very important to avoid bad outcomes.
Key Takeaways:
- Pseudomembranous colitis is a disease of the gut caused by too much Clostridium difficile bacteria after antibiotic use.
- Its signs include fever, belly pain, and diarrhea (which might be bloody or include mucus and pus).
- People over 65 or those with weak immunity, certain health problems, or gut surgeries and frequent hospital stays, are more likely to get this disease.
- It’s crucial to get diagnosed and start treatment early to prevent serious complications.
- Stem cell therapy is a new treatment that could offer hope for better outcomes in pseudomembranous colitis.
Diagnosis and Treatment of Pseudomembranous Colitis
Doctors confirm pseudomembranous colitis using various tests. These can include analyzing stool samples, blood work, and looking inside the colon. Imaging tests, like X-rays, can also provide insight.
Stool Sample Tests
Tests on stool samples are key. They check for a type of bacteria that causes the condition. By finding certain toxins, doctors can diagnose pseudomembranous colitis.
Blood Tests
High white blood cell counts in blood work can point to an infection. This suggests pseudomembranous colitis is present. So, blood tests are very important in the diagnosis.
Colonoscopy or Sigmoidoscopy
Colonoscopies and sigmoidoscopies are useful. They let doctors see the colon’s condition directly. This is done by inserting a camera-tipped tube into the colon.
Imaging Tests
In more severe cases, imaging tests might be used. They can show if the condition is getting worse. X-rays or CT scans help find any big issues, like a swollen colon.
After diagnosing pseudomembranous colitis, the focus shifts to treatment. The plan can change depending on how severe the case is and the patient’s health.
One common first step involves stopping certain antibiotics. Sometimes, doctors replace them with others that fight the infection better.
For tough cases that keep coming back or are very serious, different treatments might be needed. Fecal transplants can help by introducing healthy bacteria into the gut.
If the condition gets too risky, surgery might be the last resort. This is when the doctor has to remove the affected part of the colon.
It’s very important to catch and treat pseudomembranous colitis early. This helps prevent bad outcomes. Always see a doctor for proper diagnosis and treatment.
Prevention of Pseudomembranous Colitis
To lower the risk of pseudomembranous colitis, there are important steps to take. Drinking enough water every day is crucial. It keeps your digestive system working well and stops constipation. This, in turn, helps keep pseudomembranous colitis at bay.
Choosing the right foods can also help. Soft, easy-to-digest foods are best for managing this condition. Foods like apples, bananas, and rice can calm your stomach. They can keep the problem from getting worse. But, you should avoid things like beans, nuts, and certain veggies. These foods are hard for your body to break down. They could make pseudomembranous colitis symptoms worse.
Avoiding foods that could trigger allergies is also important. This includes staying away from fatty, spicy, and fried foods. These foods can aggravate the problem. Instead, try eating small meals more often. Doing this can help you feel better.
Following these steps can make a big difference in managing pseudomembranous colitis. Always talk to a doctor for advice that fits your specific situation. They can give you the best guidance based on your health and history.