Primary biliary cholangitis (PBC) is an autoimmune liver disease that affects more women than men. It slowly damages the small bile ducts in the liver. Over time, this can lead to cirrhosis, the failure of the liver, and even cancer. PBC is usually found in people aged 30 to 60.
Because PBC is hard to treat, there are only two main medicines that doctors use, ursodeoxycholic acid and obeticholic acid. Unfortunately, some people don’t get better with these. They might have to deal with side effects that make life hard. If PBC gets very bad, the only way to fix it is with a liver transplant.
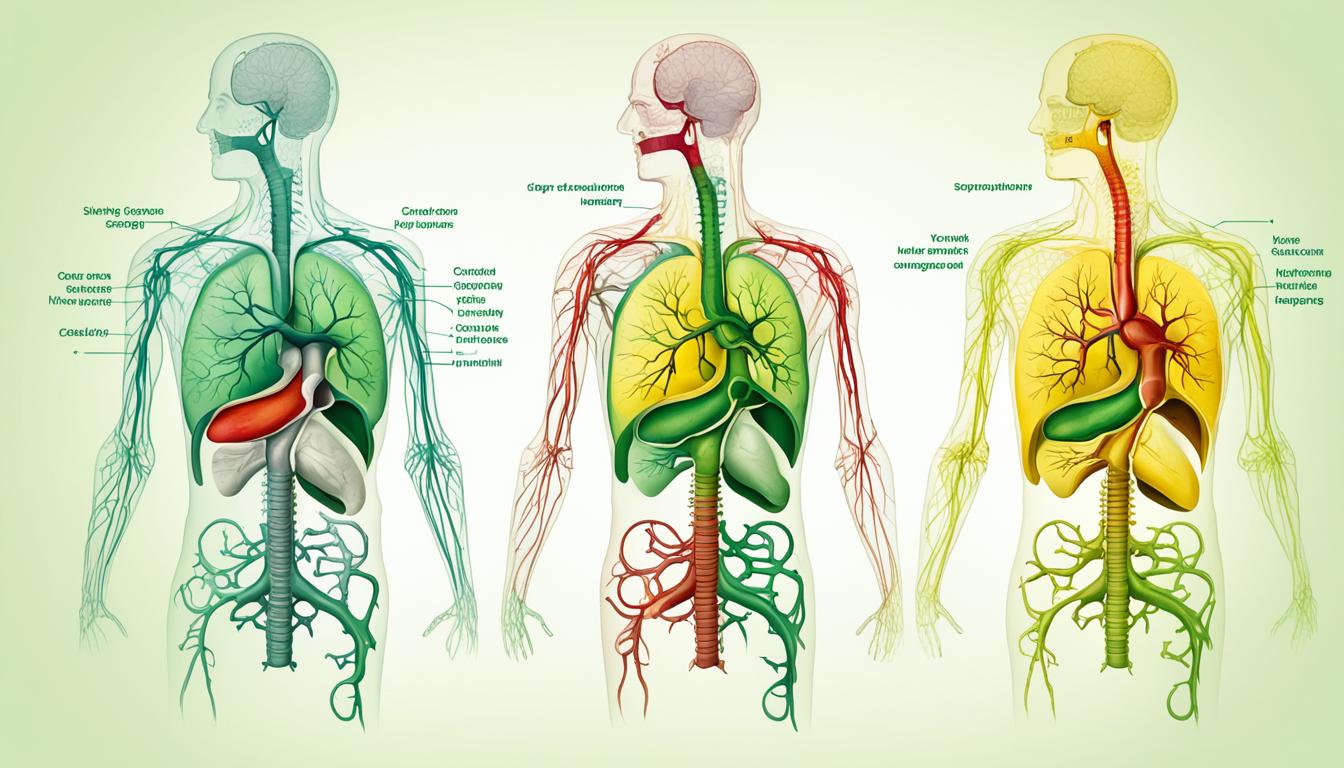
Stem cell therapy is a new and hopeful treatment for those who PBC medicines don’t help. It looks at how using special cells, Mesenchymal stem cells (MSCs), might change the disease. Doctors are studying how MSCs can maybe calm down the immune system to stop it from hurting the liver.
This article will look closely at the signs, reasons, and checks done for primary biliary cholangitis. We’ll talk about how PBC affects the liver and how using stem cells might be a big step in treating it.
Key Takeaways:
- Primary biliary cholangitis (PBC) is a cholestatic autoimmune liver disease that affects the small intrahepatic bile ducts.
- The exact cause of PBC is not fully understood, but it is believed to be an autoimmune condition where the body’s immune system attacks its own cells.
- Symptoms of PBC include fatigue, itching, dry eyes and mouth, jaundice, and abdominal pain.
- Diagnosis of PBC involves a combination of clinical presentation, laboratory tests, and imaging studies.
- Treatment options for PBC are currently limited, with ursodeoxycholic acid and obeticholic acid being the main medications used.
- For patients with end-stage PBC, liver transplantation is the only effective treatment option.
- Stem cell therapy, specifically mesenchymal stem cells (MSCs), is emerging as a potential alternative for PBC treatment, offering immunomodulation properties and the potential to repair damaged liver tissue.
Symptoms and Causes of Primary Biliary Cholangitis
Primary biliary cholangitis, or PBC, is a long-term liver issue. It happens when the bile ducts in the liver get damaged over time. This occurs because the immune system attacks the liver’s small bile ducts. This causes the ducts to become inflamed and hurts the liver.
PBC shows up more in women and usually when they’re between 30 and 60 years old. We’re not sure what exactly causes PBC. But, we think it happens because of both genetics and things in the environment.
People with PBC often feel tired and have low energy. They might also have an itch that gets worse at night. Other common signs include dry eyes and mouth, yellow skin or eyes, and pain on the right side below the ribs.
It’s vital to catch PBC early to start the right treatments and avoid more liver damage. So, if you notice any of these symptoms, go see a doctor for a checkup.
Risk Factors for Primary Biliary Cholangitis
Here’s a list of things that might make you more likely to get PBC:
| Risk Factor | Description |
|---|---|
| Gender | More common in women than men |
| Age | Most commonly diagnosed between the ages of 30 and 60 |
| Genetics | Family history of PBC or other autoimmune disorders |
| Environmental Factors | Exposure to certain chemicals or toxins |
| Autoimmune Diseases | Presence of other autoimmune conditions, such as rheumatoid arthritis or Sjögren’s syndrome |
But remember, just because you have some of these risk factors, it doesn’t mean you’ll definitely get PBC. On the other hand, you could get PBC even if you don’t have any of these risks.
Diagnosis and Treatment of Primary Biliary Cholangitis
The diagnosis of primary biliary cholangitis (PBC) requires a detailed checkup. Doctors examine signs, run lab tests, and use imaging. They look for certain indicators like anti-mitochondrial and anti-nuclear antibodies.
If your alkaline phosphatase (ALP) is high, doctors might suspect PBC. They may also perform a liver biopsy to check for damage and confirm the disease.
For treatment, ursodeoxycholic acid (UDCA) is often used first. This drug helps your liver work better, slows the disease, and can extend life.
If UDCA doesn’t work well or has side effects, obeticholic acid (OCA) is a backup. OCA can improve liver tests and how you feel.
Medication isn’t the only way to help with PBC symptoms. You might get antihistamines or bile acid sequestrants for itching. This makes life easier for PBC patients.
It’s key to stick to your treatment and have checkups with your doctor. With the right care, people with PBC can have healthier livers and better lives.
| Diagnostic Criteria for PBC | Treatment Options for PBC |
|---|---|
| – Presence of autoimmune antibodies – Elevated alkaline phosphatase levels – Liver biopsy (if needed) |
– Ursodeoxycholic acid (UDCA) – Obeticholic acid (OCA) |
| – Anti-mitochondrial antibodies (AMAs) – Anti-nuclear antibodies (ANAs) |
– Symptom management: – Antihistamines – Bile acid sequestrants |
Conclusion
Primary biliary cholangitis (PBC) is a chronic liver disease that harms the bile ducts. This can lead to serious liver issues if not treated. The good news is research is opening new doors.
Mesenchymal stem cell (MSC) therapy offers hope for those who don’t improve with regular treatments. MSCs can change how the immune system works. This can help protect the liver and maybe even fix some damage. It looks like a really promising option for PBC patients.
But, we need more studies to be sure MSC-based therapy is safe and works well for PBC. It’s not a treatment that all patients can get right now. So, until then, getting diagnosed early and proper care is key. This can help manage symptoms, slow down the disease, and keep the liver working.
In the end, fighting PBC is a big challenge that needs a team effort. Thanks to research and the potential of stem cell therapy, things are looking up for the future of PBC treatment.