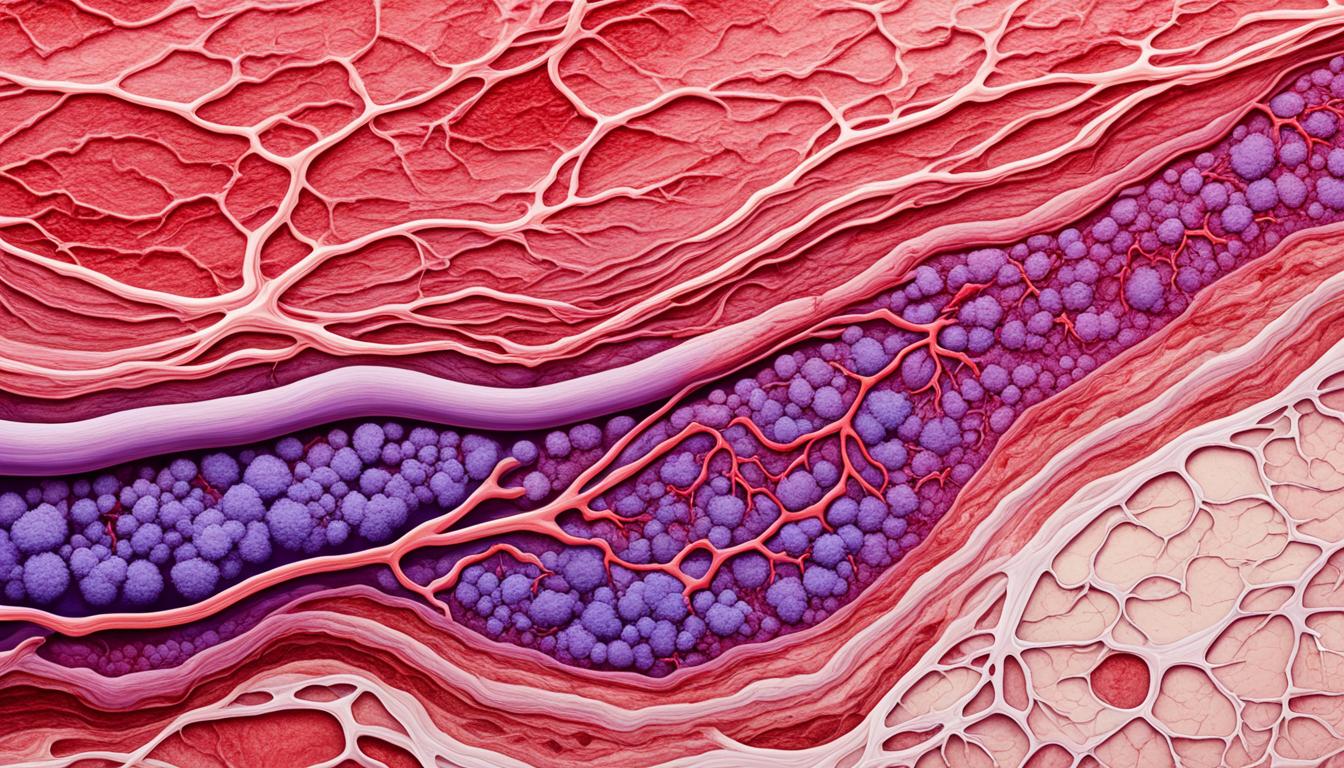
Phlebitis is when veins become swollen and painful. It leads to symptoms like pain, swelling, and redness. There are two main types: superficial which is near the skin’s surface, and deep, affecting veins inside the muscles.
Superficial phlebitis often comes from outside sources, like IVs or drugs. Deep phlebitis is linked to blood clots. Causes include trauma, infections, surgery, not moving a lot, and some illnesses.
Doctors check for phlebitis with blood tests or ultrasound. Treatments include drugs to reduce swelling, wearing support stockings, and sometimes surgery or stem cell therapy.
Key Takeaways:
- Phlebitis causes pain, swelling, and redness in the veins.
- It can be superficial (near the skin) or deep (thus affecting larger veins).
- Superficial cases often come from IVs or drugs, while blood clots cause deep phlebitis.
- Things like injuries, surgeries, and long periods without moving can raise the risk.
- Doctors might use blood tests or ultrasound to diagnose it.
- Treatments vary but can include medicine, wearing special stockings, surgery, or stem cell therapy.
Symptoms of Phlebitis
The symptoms of phlebitis differ if it’s deep or superficial. In superficial phlebitis, the vein’s area may be painful, swollen, and red. It might also feel warm to the touch and be itchy or burning. Symptoms often get worse with leg movement.
Deep phlebitis might show the same symptoms. But, some people don’t have any signs. In serious cases, you might see fever, fatigue, or have trouble breathing. If a blood clot ends up in the lungs, you could cough up blood.
Common Symptoms of Phlebitis:
- Pain along the affected vein
- Swelling and redness
- Tenderness to touch
- Warmth in the affected area
- Itching or a burning sensation
- Fever (in severe cases)
- Fatigue (in severe cases)
- Rapid heart rate (in severe cases)
- Shortness of breath (in severe cases)
- Coughing up blood (in severe cases)
If you have any of these symptoms, you must see a doctor right away. They will help with finding the cause and the right treatment.
Causes and Risk Factors of Phlebitis
Phlebitis is the inflammation of veins. It happens for many reasons and certain things make it more likely. Knowing these can help stop it early.
There are two main types: one affects the surface, the other goes deep. Superficial phlebitis can be from putting a tube in a vein or from medicines. Deep phlebitis is often caused by blood clots.
Many things can cause phlebitis, like injuries, infections, or not moving for a long time. Being careful during medical procedures and preventing phlebitis is very important. Putting a tube in or using certain drugs can lead to the surface type.
Some people are more at risk. Things like family history, hormone changes, and illness make phlebitis more likely. So does being overweight or smoking.
Preventing Phlebitis
Avoiding phlebitis is key. Regular exercise and not sitting too long help a lot. Being careful during medical treatments also reduces the risk.
It’s good to know your risks and make smart choices. For example, not smoking and keeping a healthy weight can help. So can controlling medical problems you might have.
Preventing phlebitis with a healthy lifestyle is the best approach. It keeps you from getting this disease and the problems that come with it.
| Causes of Phlebitis | Risk Factors for Phlebitis |
|---|---|
|
|
Treatment and Prevention of Phlebitis
Treating phlebitis depends on how severe and where it is. If it’s surface phlebitis, taking out what’s causing the irritation, like a catheter, is crucial. Anti-inflammatory drugs help ease symptoms. Doctors might also recommend compression stockings to boost blood flow, cutting complication risks.
Deep phlebitis needs more care to stop blood clots and dangerous issues like a pulmonary embolism. The main treatment is using blood thinners to lower clot risks. Sometimes, a surgery or putting a mesh filter in the vena cava is needed to prevent more trouble.
Preventing phlebitis means keeping healthy with regular exercise and avoiding too much sitting. Wearing compression stockings can help keep blood flowing well. It’s key to get quick help for any symptoms or injuries to stop phlebitis.