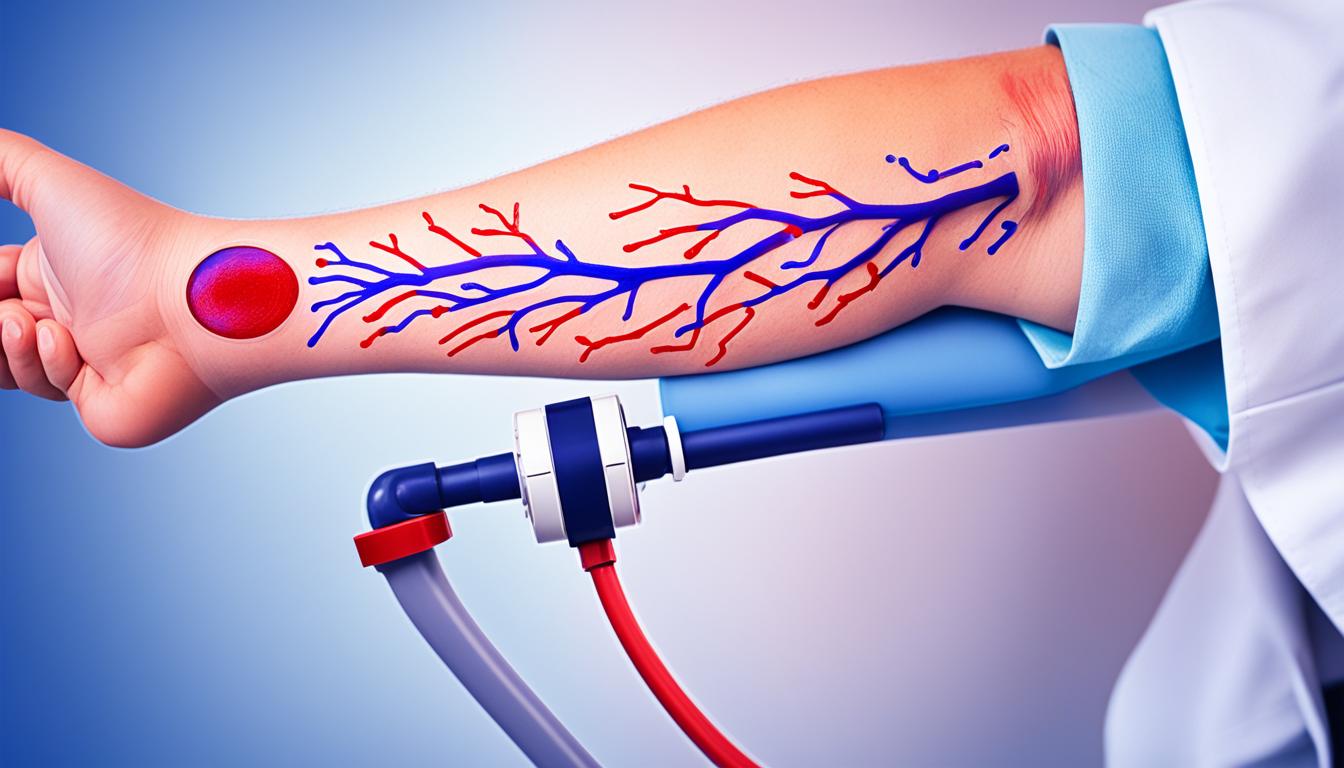
Peripheral artery disease (PAD) is a vascular disease that affects the arteries in the legs and feet. It happens when these arteries narrow or block, causing symptoms and complications. Knowing the causes, spotting the signs accurately, and considering treatments like stem cell therapy are key to living well with PAD.
The main symptom of PAD is pain in the legs, varying from slight discomfort to severe cramps. This happens because the arteries in the legs don’t carry enough blood. Often, people feel pain or cramping – a condition called claudication – when they walk or exercise.
Atherosclerosis is the leading cause of PAD. It refers to a build-up of plaque in the arteries. This plaque is made of cholesterol, fat, and other materials. It can slow down or stop blood flow, leading to blockages. Smoking, high blood pressure, diabetes, high cholesterol, and little exercise can all contribute to atherosclerosis and thus PAD.
To diagnose PAD, doctors conduct several tests and a physical review. They’ll check your medical history too. Tests such as the ankle-brachial index (ABI) measurement, Doppler ultrasound, and angiography help to see where and how severe the blockages are. This information is key in deciding the best treatment for each person.
Stem cell therapy offers new hope for PAD. It involves injecting stem cells into the problem area. Studies show this can lead to better blood flow, reduce pain, and help grow new blood vessels. This method could profoundly improve the lives of those with PAD.
Key Takeaways:
- Peripheral artery disease (PAD) causes arteries to the legs and feet to narrow or get blocked.
- Its symptoms include leg pain, poor blood flow in the lower limbs, and claudication during exercise.
- Atherosclerosis, a build-up in the arteries, is often the root of PAD.
- To diagnose PAD, doctors use tests and examine a patient’s history and condition.
- Stem cell therapy is showing promise in increasing blood circulation and reducing pain for those with PAD.
Risk Factor Modification and Medications for PAD
Making big changes to lower your risks is key in managing PAD. This means changing how you live, moving more, and taking certain medicines. Doing these things helps stop PAD from getting worse.
Risk Factor Modification
Managing PAD well starts with changing things that can be changed. This includes how we live and what we eat. Here are some main points:
- Smoking cessation: Stopping smoking is a must. It harms your blood vessels and speeds up PAD’s effects.
- Control of diabetes: Keeping blood sugar levels in check is crucial. It stops more damage to your blood vessels.
- Dyslipidemia management: Doctors might give you statins to lower bad cholesterol. This cuts your risk of heart problems.
- Hypertension control: Managing high blood pressure is vital. It lowers the chance of PAD getting worse.
- Dietary changes: Eating well helps a lot. A diet low in bad fats, salt, and cholesterol keeps you healthier.
- Regular exercise: Moving as your doctor says is good for you. It makes your heart and blood vessels stronger.
Medications for Peripheral Artery Disease Treatment
Besides changing how we live, doctors might also give us some medicines. These medicines lower our risk of heart attacks and strokes. Here’s what they might prescribe:
- Antiplatelet drugs: Medicines like aspirin keep our blood from clotting. This means fewer heart problems and strokes.
- ACE inhibitors: Drugs like lisinopril manage high blood pressure. They make our blood vessels work better.
- Statins: Medications such as atorvastatin lower bad cholesterol. This helps lessen plaque in our arteries and heart risks.
In the end, treating PAD requires big lifestyle shifts and keeping risk factors low. Moving more and eating well are crucial. Plus, medicines help prevent heart issues in people with PAD.
Treatment Options for Severe PAD
When peripheral artery disease (PAD) gets severe, it might not improve with common treatments. Yet, there are still methods to help. These include percutaneous transluminal angioplasty (PTA), surgery, and even stem cell therapy. The goal of each of these is to ease symptoms and improve the life of someone with severe PAD.
Percutaneous Transluminal Angioplasty (PTA)
Percutaneous transluminal angioplasty (PTA) doesn’t require surgery. It helps open up blocked or narrow blood vessels. A catheter with a balloon tip is used. When the balloon inflates, the vessel widens, improving blood flow. Sometimes, a stent is placed to keep the artery open.
Surgical Interventions
When PTA isn’t an option, surgery can be considered. For example, a surgery called thromboendarterectomy removes plaque from the artery. This helps blood flow better. Another surgery, like femoropopliteal bypass, creates a new path for blood to go around a blocked area.
Amputation
Amputation becomes necessary if severe PAD causes infection or gangrene. It’s usually the last choice when other treatments don’t work.
Stem Cell Therapy
Stem cell therapy shows promise for severe PAD. It uses the patient’s own stem cells, often from their bone marrow. These cells can encourage new blood vessels to grow. This improvement in blood flow can lower the need for amputation.
More studies are needed to confirm how well stem cell therapy works for severe PAD. Yet, it could be a way to avoid amputation in the future. The goal is to fully understand and use this therapy effectively.
Conclusion
Peripheral artery disease (PAD) makes legs hurt and blood flow lower because of blocked arteries. It’s important to change risk factors, exercise, and take medicine to handle PAD. In severe instances, treatments like percutaneous transluminal angioplasty (PTA), surgery, or amputation may be needed.
There’s hope in new options like stem cell therapy for PAD. Research shows stem cells might boost leg blood flow and cut down pain in PAD patients. But, we still need more studies to fully understand how well it works and its lasting effects.
Quick diagnosis and the right treatment are key to PAD management and bettering life for those with it. By tackling risk factors, doing advised exercises, using prescribed drugs, and considering treatments, PAD symptoms can be eased. This helps improve leg blood flow and lets people take back control of their lives.