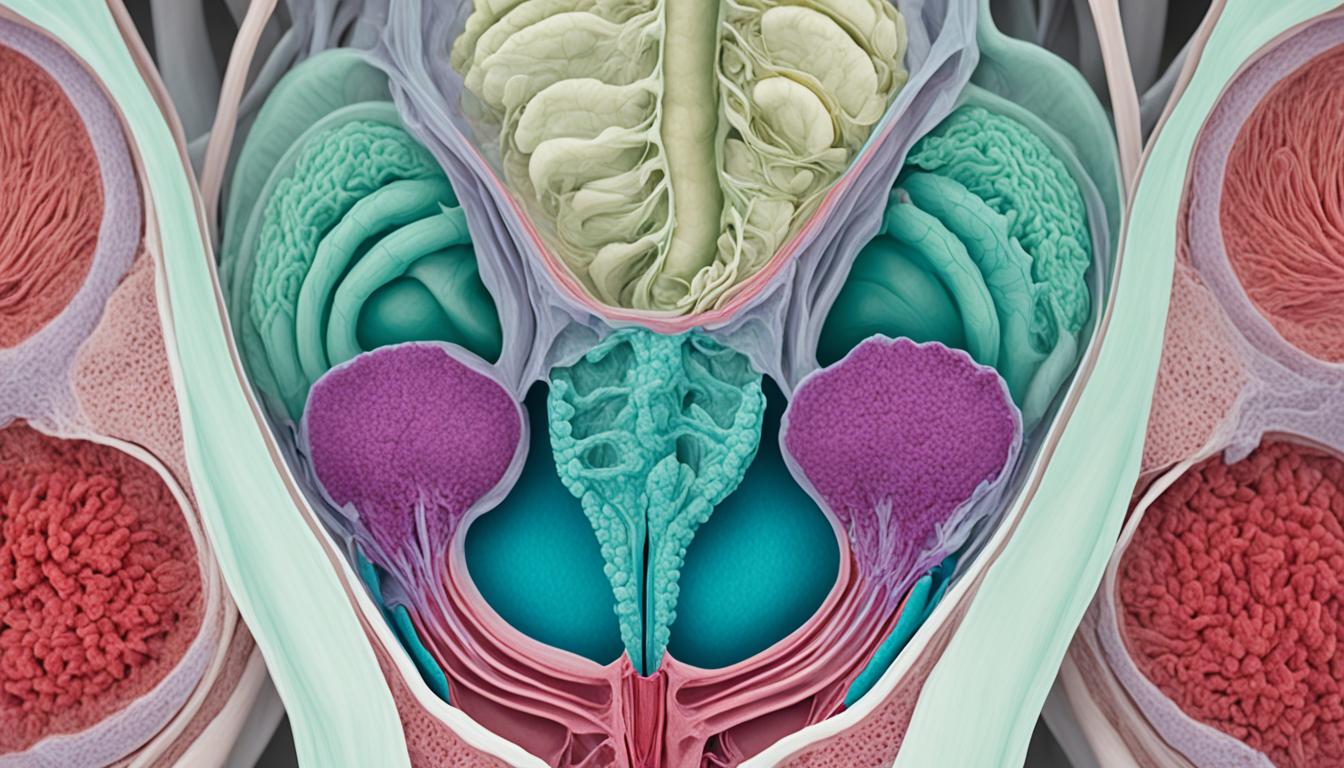
Pelvic organ prolapse is more common in women after vaginal childbirth. It occurs when vital structures that hold up the pelvic organs weaken. This makes the organs shift into or outside the vagina, which is known as uterine prolapse.
Symptoms can include feeling a bulge in the pelvic area and discomfort in the vagina. Women might also experience urine leaks, find it hard to empty their bladder, and feel pain during sex. Lower back or pelvic pain are also signs.
Several factors can lead to uterine prolapse. Vaginal births, especially many, can weaken the pelvic muscle and tissues. Others include hormonal changes in menopause, getting older, and health issues like obesity or chronic coughs.
Doctors diagnose uterine prolapse by checking medical history, doing physical exams, and using imaging tests. They also assess the muscles that support the pelvic floor. Treatment might involve exercises, lifestyle changes, and using pessaries, but surgery could be an option in severe cases.
While still under research, stem cell therapy could be a future treatment. The idea is to use a woman’s own stem cells to repair the damaged tissue. It’s being studied with a plant-based product, such as an aloe vera hydrogel. Yet, these studies are still in the early stages and have not been tested on humans.
Key Takeaways:
- Pelvic organ prolapse, specifically uterine prolapse, occurs when the tissues supporting the pelvic organs become damaged or weakened.
- Symptoms of uterine prolapse include a bulging sensation in the pelvic area, discomfort or pressure in the vagina, urinary incontinence or frequent urination, difficulty emptying the bladder, pain or discomfort during sexual intercourse, and lower backache or pelvic pain.
- Main causes of uterine prolapse are vaginal delivery, hormonal changes during menopause, aging, obesity, and chronic conditions like chronic coughing.
- Diagnosis of uterine prolapse involves medical history evaluation, physical examinations, imaging tests, and pelvic floor assessments.
- Treatment options for uterine prolapse include non-surgical approaches like pelvic floor exercises, lifestyle modifications, and the use of pessaries. Surgical interventions may be necessary in severe cases.
- Stem cell therapy using a woman’s own endometrial stem cells delivered in a plant-based product is being explored for uterine prolapse, but it is still in the experimental stage and not ready for human clinical trials.
Causes, Risk Factors, and Diagnosis of Pelvic Support Problems Uterine Prolapse
Uterine prolapse, a type of pelvic organ prolapse, happens because of many causes and risk factors. Knowing these factors well is crucial for proper diagnosis and treatment.
Causes of Uterine Prolapse
The main cause of uterine prolapse is the weakening of muscles and tissues. These support the pelvic organs. Several key factors lead to this weakening:
- Vaginal delivery puts pressure on the pelvic floor. This can weaken it, especially after multiple births, causing uterine prolapse.
- Menopause brings hormonal shifts that affect pelvic tissue strength and elasticity, leading to prolapse.
- As women grow older, their muscles, including pelvic floor muscles, naturally get weaker. This contributes to uterine prolapse.
- Chronic health issues and lifestyle choices like chronic coughing, obesity, and heavy lifting can strain the pelvic floor. This greatly increases the risk of prolapse.
Diagnosis of Uterine Prolapse
An accurate diagnosis is key for the right treatment of uterine prolapse. The process for diagnosis usually includes several steps:
- The doctor will first look at the medical history. They will check for symptoms or risks that could lead to prolapse.
- A physical exam, like a pelvic exam, is performed. This checks the pelvic organs and tissues’ health and strength.
- Imaging tests, like ultrasounds or MRIs, can offer detailed pictures. These help see the prolapse’s extent and find any other problems.
- Pelvic floor assessments test the muscles. They check the pelvic floor’s strength and function. This is crucial for deciding on the best treatment.
By using these diagnostic tools together, doctors can pinpoint uterine prolapse. They then tailor a treatment plan to meet each patient’s specific needs.
Advancements in Stem Cell Therapy for Pelvic Support Problems Uterine Prolapse
Scientists are looking into how stem cell therapy for uterine prolapse can work. They’re focusing on endometrial stem cells from a woman’s own body. These cells could be used with a aloe vera hydrogel delivery system. The goal is to help heal and grow tissue back.
This method is new and hopes to fix the pelvic floor after childbirth. It’s not ready for people yet, but it might avoid the need for surgery for pelvic organ prolapse. By using endometrial stem cells with aloe vera gel, they want to lower surgery needs after childbirth.
Key scientists from the Hudson Institute, working with Monash University and the Melbourne Centre for Nanofabrication are leading the way. Even though tests on people haven’t started, this approach looks very promising. It could help many women who have pelvic floor and uterine problems.