Popliteal Artery Entrapment Syndrome (PAES) is a rare issue that affects how blood flows in the legs. It happens when a leg artery is squeezed by nearby muscle or tendons. This can be from birth or begin later in life.
Young athletes who do intense sports like running, cycling, or weightlifting are more likely to get PAES. The top symptom is pain in the back of the leg, often during or after activity. Other signs include cold feet, numbness, and changes to skin color.
Doctors use tests like ultrasound, MRI, or CTA to check for PAES. These show how much the artery is blocked and how well blood flows through it.
Surgery is the main treatment to fix PAES by releasing the tight artery. In some cases, bypass surgery might be needed. Stem cell therapy is a new idea for treating PAES. It aims to repair tissues and help with blood flow, making things better for the patient.
Key Takeaways:
- PAES is a rare condition that affects leg blood flow.
- The main symptom is calf pain, but other signs like cold feet can happen too.
- Doctors find PAES using exams like ultrasound or MRI.
- Treatments include surgery to fix the artery and stem cell therapy to help heal the area.
- Getting diagnosed early and treated right can prevent more serious issues and boost life quality.
What is Popliteal Artery Entrapment?
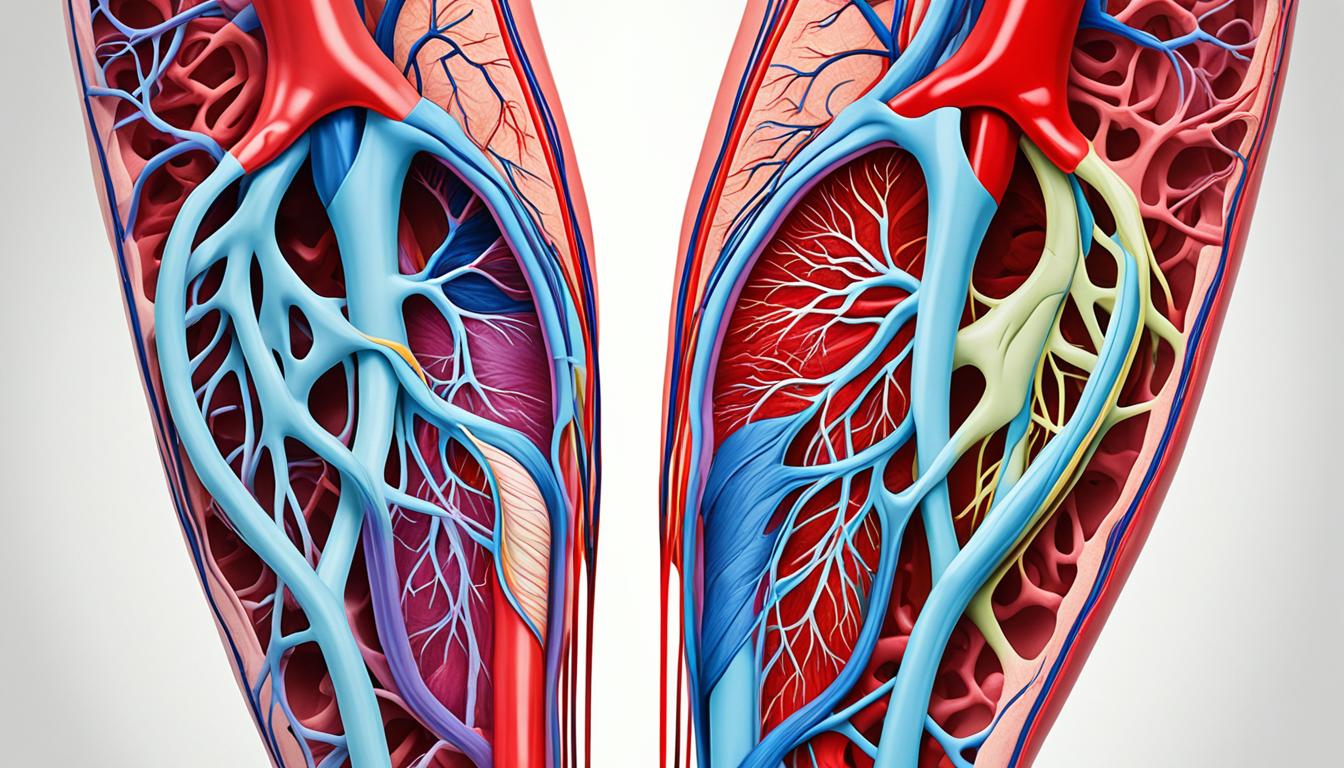
The popliteal artery carries blood from the heart to the legs. In most people, it works well without problems from the calf muscles. But in Popliteal Artery Entrapment Syndrome (PAES), the artery gets squeezed by the calf muscle.
This squeezing slows blood flow to the lower leg, leading to leg issues. PAES might be from birth (congenital) or appear later (acquired). With congenital PAES, the muscle or artery grew in a strange way before birth. Acquired PAES happens when the muscle grows too big because of sports or muscle training.
Comparison of Congenital and Acquired Popliteal Artery Entrapment
| Congenital PAES | Acquired PAES |
|---|---|
| Present at birth | Develops later in life |
| Abnormal positioning during fetal development | Associated with hypertrophied calf muscles due to high-stress activities |
Symptoms, Risk Factors, and Diagnosis of PAES
Popliteal Artery Entrapment Syndrome (PAES) shows several symptoms. These signs help doctors spot and diagnose PAES. The main symptom is pain or cramps in the lower leg’s back, specifically in the calf. This discomfort happens during physical activities or while resting. It might be ongoing or come and go.
PAES might also cause cold feet after physical activity and numbness in the calf. Other signs include cramps at night and changes in the skin color around the calf muscles. These are hints of poor blood flow in the lower leg, a common issue with PAES.
The chance of having PAES is higher for young males and those in demanding sports. It’s often seen in runners, cyclists, and weightlifters. These sports require a lot of effort from the leg muscles.
To diagnose PAES, a doctor will check your symptoms and do a careful physical exam. They will focus on your calf muscles, check muscle strength, and look for pulses in your legs.
Diagnostic Imaging Techniques
Several tests are used to confirm PAES and to see how serious it is. These tests include:
- Ultrasound: It creates images of blood vessels with sound waves. It’s used to check the flow of blood and spot issues in the popliteal artery.
- Magnetic Resonance Imaging (MRI): MRI creates detailed images of the inside of your body with magnets and radio waves. It shows the popliteal artery clearly, which helps doctors check for any blockages.
Using these tests together helps doctors find out if you have PAES. They can also plan the best way to treat it.
| Diagnostic Techniques | Advantages | Disadvantages |
|---|---|---|
| Ultrasound | Non-invasive, real-time visualization of blood flow | Operator-dependent, limited in obese individuals |
| Magnetic Resonance Imaging (MRI) | Highly detailed imaging, no radiation exposure | Expensive, time-consuming, contraindicated for individuals with certain implants or pacemakers |
Treatment Options for PAES
PAES is mostly treated with surgery to fix the main issue. This surgery is called popliteal artery release. It helps by moving a calf muscle that presses on the artery. By doing this, blood flow to the leg improves, and symptoms lessen.
If PAES is really bad or has been there for a long time, a bypass surgery might be needed. This surgery directs blood around the blockage. It’s used when just moving the muscle isn’t enough to fix the issue.
There’s also an exciting treatment called stem cell therapy for PAES. Stem cells, injected into the leg, help grow new tissue and boost blood flow. This new treatment can help reduce symptoms and improve how the leg works.
Getting diagnosed early and treating PAES soon is very important. So, if you have signs like calf pain, cramps, cold feet, or skin color changing, see a doctor. They’ll check and choose the best treatment, which could be surgery, stem cell treatment, or a mix of both, just for you.