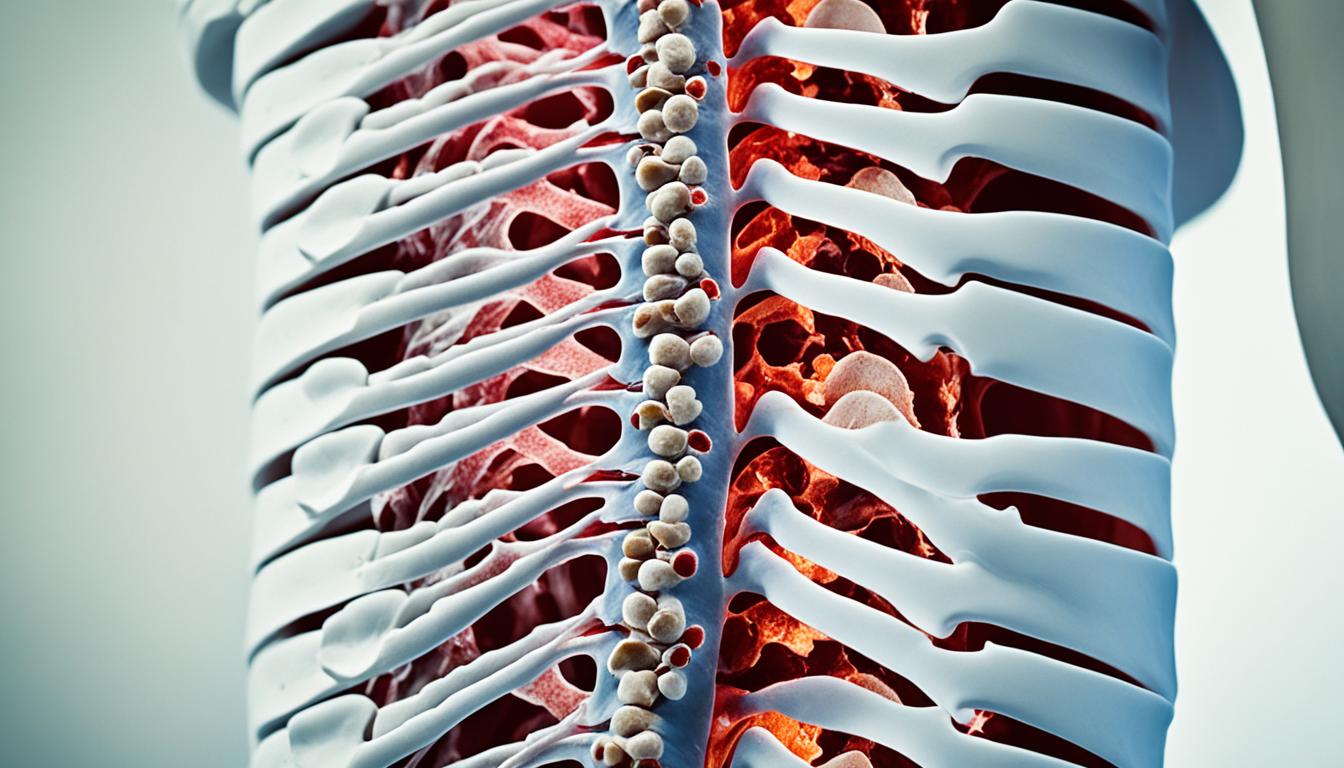
Osteophytes, also called bone spurs, are common in aging spines. They arise due to degenerative changes and increased joint forces. These non-cancerous growths protrude from osteoarthritic joints’ margins.
They consist of newly formed fibrocartilage and bone, typically at joints’ edges. Cartilage meets the periosteum at these locations. Osteophytes develop through stem cells’ chondrogenic differentiation, often originating from the periosteum.
This may be cells’ repair response to altered growth factors after joint injury. In some cases, osteophytes can contribute to affected joints’ stability.
Key growth factors involved include TGF-β superfamily members, bone morphogenetic proteins (BMPs), insulin-like growth factor (IGF), and fibroblast growth factor (FGF).
Key Takeaways
- Osteophytes, or bone spurs, are non-cancerous growths at osteoarthritic joints’ margins.
- They consist of newly formed fibrocartilage and bone at cartilage-periosteum interfaces.
- Formation is believed to be a cellular repair response after joint injury.
- Growth factors like TGF-β, BMPs, IGF, and FGF enhance stem cell differentiation into osteophytes.
- In some cases, osteophytes may contribute to affected joints’ stability.
Understanding Osteophytes
Osteophytes are bony projections resulting from abnormal bone growth. They commonly occur in degenerative spines. In the cervical spine, osteophytes develop due to uneven pressure on vertebral endplates and facet joints. This pressure arises from intervertebral disc degeneration.
Osteophytes are a cellular repair response to altered growth factors after joint injury. They form through chondrogenic differentiation of progenitor cells, often from the periosteum. This leads to new fibrocartilage and bone formation at joint peripheries, typically between cartilage and periosteum.
Definition and Formation
Three types of osteophytes exist based on shape and location: traction osteophytes, claw osteophytes, and wraparound bumper osteophytes. Imaging techniques like MRI identify osteophytes, though distinguishing them from disc herniations can be difficult. Specialized techniques like SW-MRI provide better differentiation by conveying a hyperintense signal to calcified structures like osteophytes.
Osteophytes
Symptoms
Patients with symptomatic osteophytes often describe stiffness in the neck, mid, or lower back. This stiffness may be associated with a dull ache and possibly lack of mobility or range of motion.
The lack of mobility is often noted in the neck and lower back when patients attempt to bend forwards, backwards, or rotate left or right.
Depending on the extent and location of the bone spur, the nerves branching off the spinal cord may be affected. If this happens, patients may experience radicular symptoms like pain, numbness, or tingling radiating into the arms or legs.
Causes and Risk Factors
Osteophytes commonly result from degenerative changes and increased forces on the joints. Contributing factors include age, obesity, joint injury, and certain medical conditions like osteoarthritis and rheumatoid arthritis.
Diagnosis
Accurate diagnosis of osteophytes is crucial for developing an appropriate treatment plan. Imaging tests like X-rays, MRI, and CT scans identify the presence and extent of osteophytes.
These diagnostic tools help differentiate osteophytes from other spinal conditions, such as disc herniations.
Conclusion
In summary, osteophytes, or bone spurs, are common as the spine ages. They often result from degenerative changes and increased joint forces. Their presence doesn’t necessarily cause pain directly. However, they can be linked to spinal conditions causing stiffness, reduced mobility, and radiating pain.
Accurate diagnosis through imaging tests like X-rays, MRIs, and CT scans is crucial. This helps develop an appropriate treatment plan involving conservative, non-surgical approaches initially. More advanced interventions like stem cell therapy may be considered later.
Understanding the root causes and risk factors for osteophyte formation is key. By addressing these underlying causes and implementing a comprehensive strategy, individuals can find relief. They can maintain overall spinal health and mobility. With medical advancements and innovative therapies like stem cell therapy, managing osteophytes is becoming more promising.