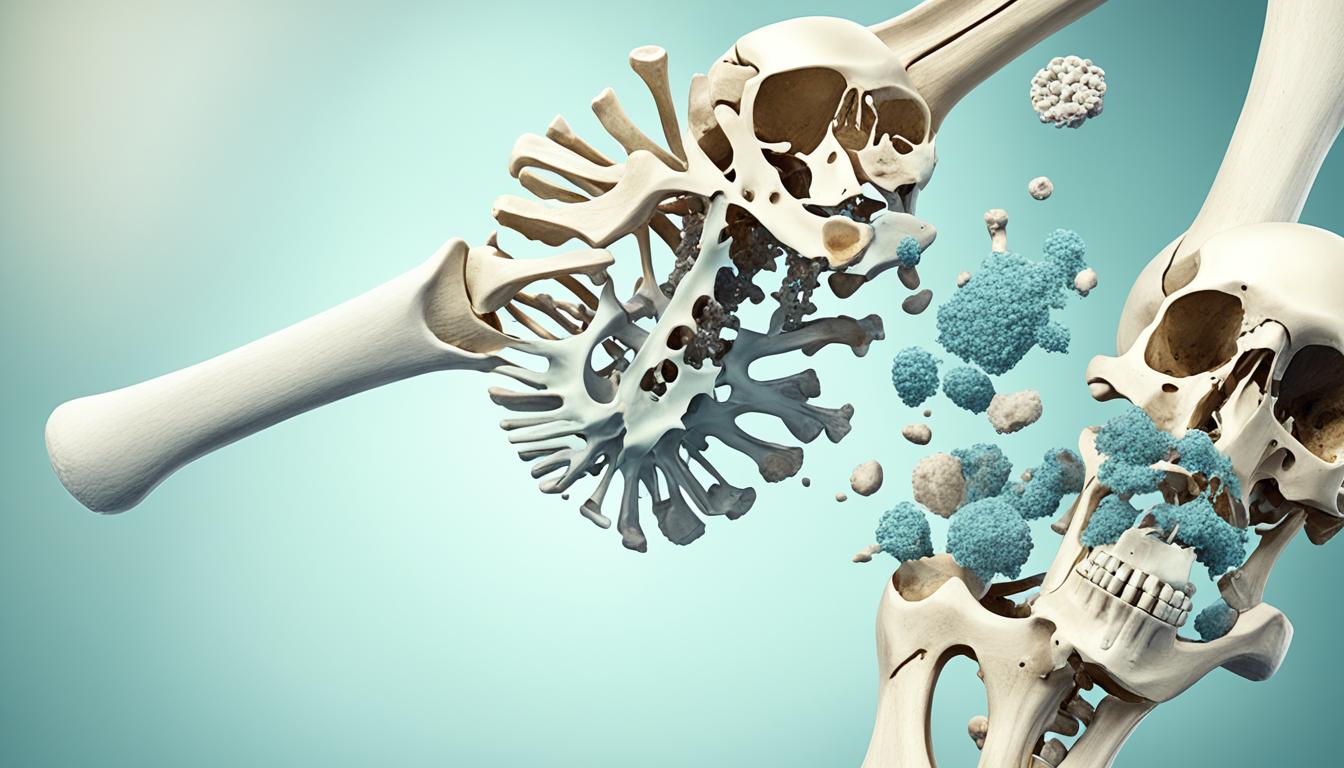
Osteonecrosis, known as avascular necrosis (AVN), is a disease causing bone cells to die. If bones near a joint are affected, the joint surface often collapses, leading to arthritis due to an irregular surface.
It commonly affects long bone ends like the femur (thigh), upper femur (hip ball), lower femur (knee), upper humerus (shoulder), and ankle bones. Osteonecrosis can affect one bone, multiple bones simultaneously, or different bones over time.
Orthopedic surgeons diagnose it using X-rays or MRI scans. The disability depends on the affected area, size, progression, and bone’s rebuilding effectiveness. Untreated, the bone may crack, compress, develop an irregular joint surface, causing arthritic pain and loss of function.
Key Takeaways
- Osteonecrosis is a bone disease that can lead to joint collapse and arthritis.
- It commonly affects the hip, knee, shoulder, and ankle joints.
- Early symptoms may be mild, but the disease can progress to severe joint pain and disability.
- Causes include injury, medications, alcohol abuse, and certain medical conditions.
- Treatment aims to prevent further bone damage and may involve various therapies and surgical options.
Understanding Osteonecrosis
Osteonecrosis is a bone disease. It causes bone tissue death due to lack of blood supply. Bones are living cells that require healthy blood flow. In osteonecrosis, blood flow disrupts, leading to bone tissue death.
Bone breakdown and joint collapse can eventually occur.
Definition and Overview
Osteonecrosis is a condition where bone tissue dies due to interrupted blood supply. It commonly affects long bone ends like the thigh bone (femur) – upper part (hip socket ball) and lower end (knee joint part).
The upper arm bone (humerus) – upper part (shoulder joint ball) is frequently affected too. Osteonecrosis involving a joint bone part can lead to bone breakdown and arthritis development.
Commonly Affected Bones
Osteonecrosis often affects long bone ends like the femur (thigh bone) and humerus (upper arm bone). Areas commonly involved include:
- Upper femur – hip socket ball
- Lower femur – knee joint part
- Upper humerus – shoulder joint ball
Osteonecrosis involving a joint bone part can lead to bone breakdown and arthritis development.
Osteonecrosis: Symptoms and Causes
Osteonecrosis may not show early signs. As it progresses, most patients feel joint pain. Initially, pain occurs only when weight is put on the affected joint. Eventually, it may persist even at rest.
The pain develops gradually, ranging from mild to severe. If osteonecrosis advances and bone/joint surface collapses, pain may increase dramatically. Joint stiffness and limited range of motion in the affected area may occur. Disabling osteoarthritis may also develop.
Risk Factors and Causes
Osteonecrosis can have various causes, like injury (bone fractures or joint dislocations), certain medications (corticosteroids), excessive alcohol use, and medical conditions. These conditions include Gaucher disease, pancreatitis, autoimmune disorders, cancer, HIV infection, decompression disease, and blood disorders like sickle cell disease.
In some cases, the exact reason for osteonecrosis development is unknown (idiopathic).
| Osteonecrosis Risk Factors | Osteonecrosis Causes |
|---|---|
| Injury (bone fracture or joint dislocation) | Medications (corticosteroids) |
| Excessive alcohol use | Gaucher disease |
| Autoimmune disorders | Pancreatitis |
| Cancer | HIV infection |
| Decompression disease | Sickle cell disease |
| Idiopathic (unknown cause) | – |
The exact mechanisms by which some risk factors and causes lead to osteonecrosis development are not fully understood. Further research is needed to uncover the underlying processes involved.
Conclusion
The primary aim in treating osteonecrosis is preventing further bone deterioration. In early stages, medications like NSAIDs, osteoporosis drugs, cholesterol-lowering drugs, and vasodilators may alleviate symptoms.
Rest, exercises, and electrical stimulation therapies may also help early-stage patients.
For advanced cases, surgical interventions like core decompression, bone transplant, bone reshaping, and joint replacement may become necessary.
A newer regenerative treatment using stem cell therapy with bone marrow aspirate and concentration has shown promise in early-stage osteonecrosis of the hip. However, more research is still needed.
With proper, timely treatment, osteonecrosis progression can halt, preventing bone damage and joint collapse. This improves patients’ quality of life and mobility.
While challenging, advancements in medical and surgical osteonecrosis treatments offer hope.