Osteoarthritis is a degenerative condition affecting joints. It causes pain, swelling, and stiffness. It impacts a person’s ability to move freely.
Osteoarthritis is the most common joint disorder. Symptoms often appear in the 40s and 50s. Nearly everyone experiences it by age 80.
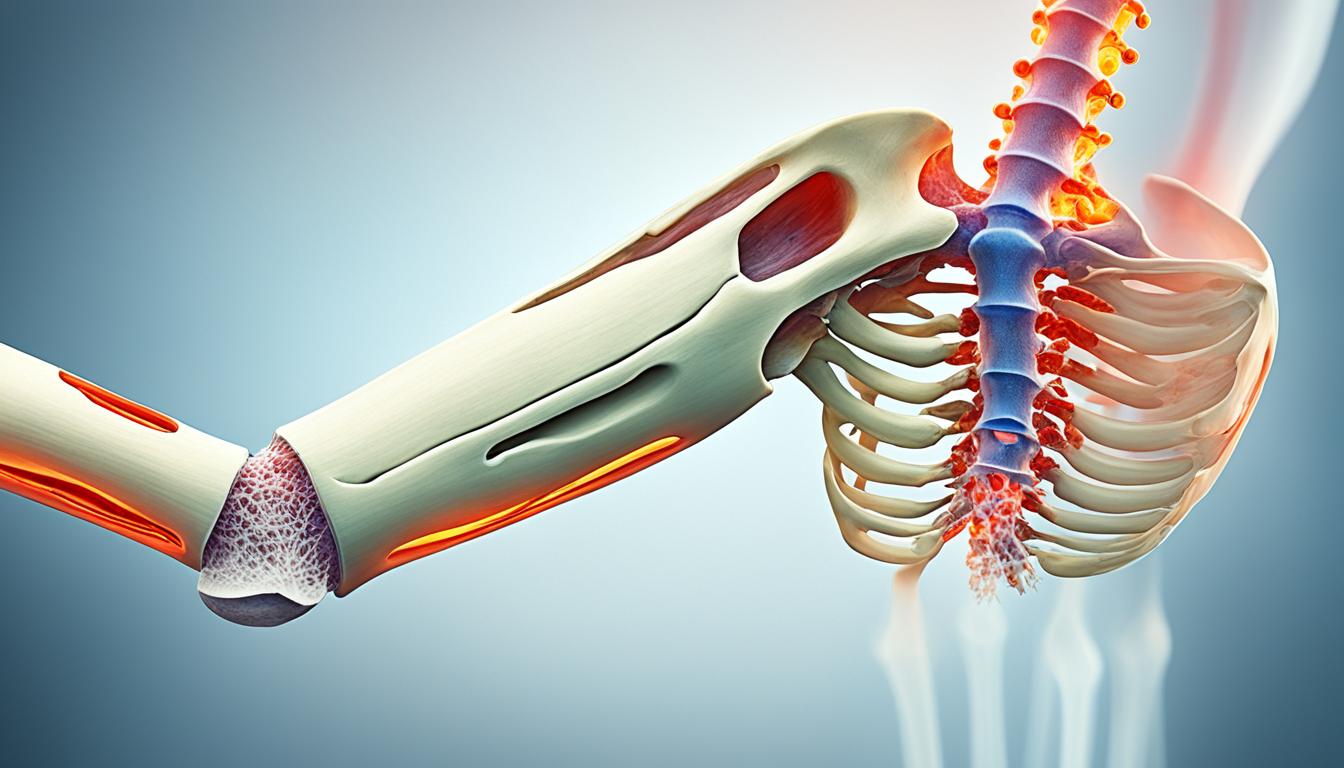
Osteoarthritis primarily damages joint cartilage. This leads to pain, swelling, and joint stiffness.
Key Takeaways
- Osteoarthritis is a prevalent and debilitating joint condition. It can significantly impact an individual’s quality of life.
- The primary symptoms are pain, swelling, stiffness, and difficulty moving the affected joint.
- Osteoarthritis damages joint cartilage, leading to pain, swelling, and joint stiffness.
- While there is no cure, a multifaceted approach can alleviate symptoms and slow progression.
- Stem cell therapy aims to regenerate damaged joint tissue and improve overall joint function.
Understanding Osteoarthritis
Osteoarthritis is a chronic condition. It’s known as degenerative joint disease. Cartilage in joints gradually deteriorates. This leads to pain, swelling, and stiffness around affected joints. It interferes with moving freely and daily activities.
Definition and Overview
Osteoarthritis is a degenerative, chronic joint disease. It primarily damages joint cartilage. This causes distortion of joint tissues. The entire joint is affected, including surrounding tissues. It’s commonly seen in knees, hips, spine, and hands.
Prevalence and Risk Factors
Osteoarthritis is the most prevalent arthritis type. Millions worldwide are affected. Its prevalence increases with age. Nearly everyone has it by 80. Several risk factors exist, like obesity, joint injury, genetics, and metabolic disorders.
Osteoarthritis Symptoms and Diagnosis
Osteoarthritis is a complex condition. It can present a wide range of symptoms and signs. Understanding these is crucial for timely diagnosis and effective disease management.
Signs and Symptoms
The primary osteoarthritis symptoms include pain, swelling, stiffness, and joint movement difficulty. These often develop gradually, though they can start abruptly after injury or strain. Osteoarthritis commonly affects knees, hips, spine, and small hand joints. It leads to reduced mobility and decreased muscle strength due to decreased joint movement.
In addition, individuals may experience general joint tenderness, crepitus (crackling or grinding sound during movement), and decreased range of motion. Osteoarthritis progression is chronic and gradual, with worsening symptoms over time.
Diagnostic Methods
Diagnosing osteoarthritis typically involves clinical assessment, medical history, and various diagnostic methods. Healthcare providers may utilize the following tools:
- Physical examination: Assessing affected joint(s) for swelling, tenderness, and limited range.
- Imaging tests: X-rays, MRI, or CT scans visualize joint damage like cartilage loss, bone spurs, and joint space narrowing.
- Laboratory tests: Blood tests rule out conditions like rheumatoid arthritis or gout with similar symptoms.
Combining medical history, physical examination, and diagnostic tests, providers can accurately diagnose osteoarthritis. They develop personalized treatment plans to manage the condition and improve patient’s quality of life.
Conclusion
Osteoarthritis significantly impacts one’s quality of life. While no cure exists, a multifaceted approach helps manage symptoms. Osteoarthritis treatment and osteoarthritis management strategies like therapy, weight control, and anti-inflammatory drugs effectively manage the condition.
Osteoarthritis stem cell therapy shows promise in regenerating cartilage and reducing inflammation. It offers potential for targeted, personalized treatment approaches. As research advances, providers and patients can explore options.
A comprehensive, patient-centered approach empowers individuals to actively manage osteoarthritis. Evidence-based interventions and professional support help maintain mobility and independence, enhancing joint health and overall well-being.