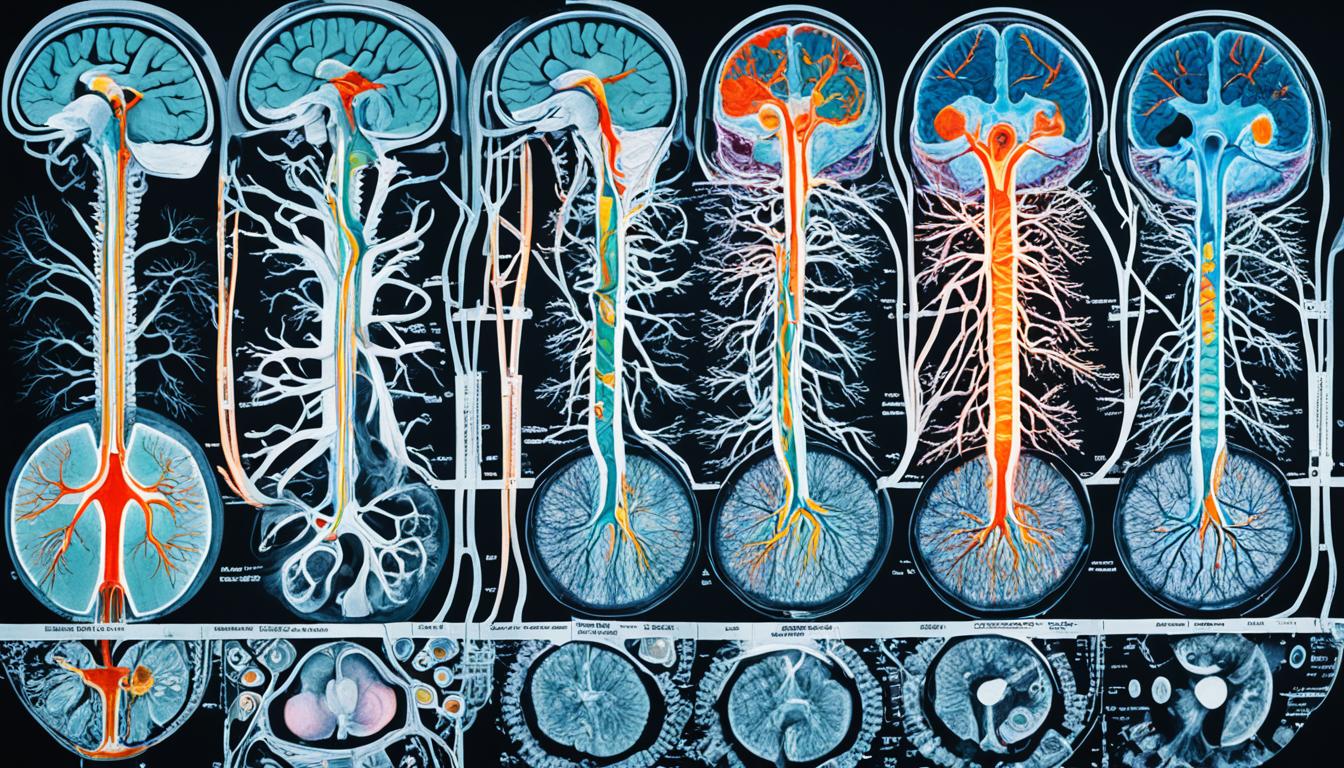
Neuromyelitis optica (NMO) is a rare autoimmune disease. It targets the optic nerves and spinal cord. This can lead to sight loss and other problems. People with NMO have attacks that last from days to months. These attacks can cause serious, long-lasting damage. Symptoms may include vision problems, muscle weakness, and issues with the brain’s normal functioning.
One key sign of NMO is optic neuritis. It can make your eyes hurt and your vision blurry. It can also cause part of your vision to disappear. This makes it hard to see in the dark. Another common symptom is myelitis. This can lead to muscle weakness or paralysis.
NMO happens when the immune system attacks the body by mistake. There are two forms of this attack: one involving AQP4 antibodies and one involving MOG antibodies. Scientists are still studying the exact cause. They believe a mix of genetic and environmental factors might play a part. If you have other autoimmune diseases or inflammatory conditions, you could be at risk for NMO.
To diagnose NMO, doctors look at your symptoms, your health history, and do tests. They’ll check for optic neuritis and myelitis. A blood test can show if you have AQP4 antibodies. Other tests like MRIs and spinal taps help confirm the diagnosis.
Treating NMO focuses on easing symptoms and avoiding future attacks. During attacks, you might get high-dose steroids to lower inflammation. Immunosuppressive drugs can help control your immune system in the long run. In rare, severe cases, plasma exchange might be needed. Stem cell therapy is in the research phase as a possible future treatment.
Research on NMO is ongoing. Scientists want to better understand the disease and find better treatments. They’re studying specific antibodies linked to NMO. They’re looking into new drugs and treatments, including stem cell therapy.
In conclusion, NMO is a serious disease that needs early diagnosis and proper treatment. There’s hope for better therapies in the future. Ongoing research is key to improving care for NMO patients.
Key Takeaways:
- NMO is a rare autoimmune condition that causes symptom “attacks” lasting from days to months.
- Primary symptoms include optic neuritis, myelitis, and brain function disruptions.
- NMO is diagnosed based on clinical symptoms, medical history, physical examination, and laboratory tests.
- Treatment options include high-dose corticosteroids, immunosuppressive medications, plasma exchange, and stem cell therapy.
- Ongoing research aims to deepen understanding, develop more effective treatments, and improve care for individuals with NMO.
Diagnosis and Treatment of NMO
Neuromyelitis optica (NMO) is found through a thorough assessment. This includes symptoms, personal health story, and tests. A diagnosis of NMO needs optic neuritis, myelitis, and specific images. These show it’s NMO and not something else.
To confirm NMO, doctors often check for AQP4 antibodies in the blood. If these antibodies show up, it strongly points to NMO. Doctors may also use MRI, a spinal tap, and other tests to be sure.
The goal in treating NMO is to manage symptoms, avoid new incidents, and limit any disability. For sudden attacks, patients might get high-dose steroids. Medicines that calm the immune system, like azathioprine and mycophenolate mofetil, are also used.
If NMO is very severe, and standard treatments don’t help, plasmapheresis could be tried. This involves cleansing the blood to reduce harmful antibodies and substances.
An exciting area for NMO treatment is stem cell therapy. This treatment aims to reset the immune system. Researchers are studying its effectiveness.
Continued care with a team of experts is vital for NMO management. Neurologists and eye doctors are key members. They watch for changes, tweak treatments, and manage any issues.
Common Medications Used in the Treatment of NMO
| Medication | Usage |
|---|---|
| Azathioprine | To suppress the immune system and prevent relapses |
| Mycophenolate Mofetil | To reduce immune activity and control disease progression |
| Rituximab | To target and deplete specific immune cells involved in NMO |
| Eculizumab | To inhibit the complement system and reduce inflammation |
Current Research and Future Perspectives
Scientists are hard at work studying NMO to better understand it and find improved treatments. They are looking closely at aquaporin-4 and myelin oligodendrocyte glycoprotein. These could hold the keys to better treatments for NMO.
There is exciting progress in finding new ways to fight NMO. Monoclonal antibodies, designed to block aquaporin-4, and other immune treatments show hope in tests. Also, stem cell therapy might be a game-changer for NMO. Tests are seeing if putting hematopoietic stem cells back can help.
The future of NMO treatment is bright. Personalized medicine may change things by tailoring treatments to each person’s immune system. This could lead to better outcomes for those with NMO. Many clinical trials are happening. They are testing new therapies to try and improve care for NMO patients.
The NMO community, including patients, family, and friends, is essential. Their support and advocacy help move research forward. It’s important for people with NMO to keep up with the current research. They should work closely with their healthcare team for the best management of their condition.