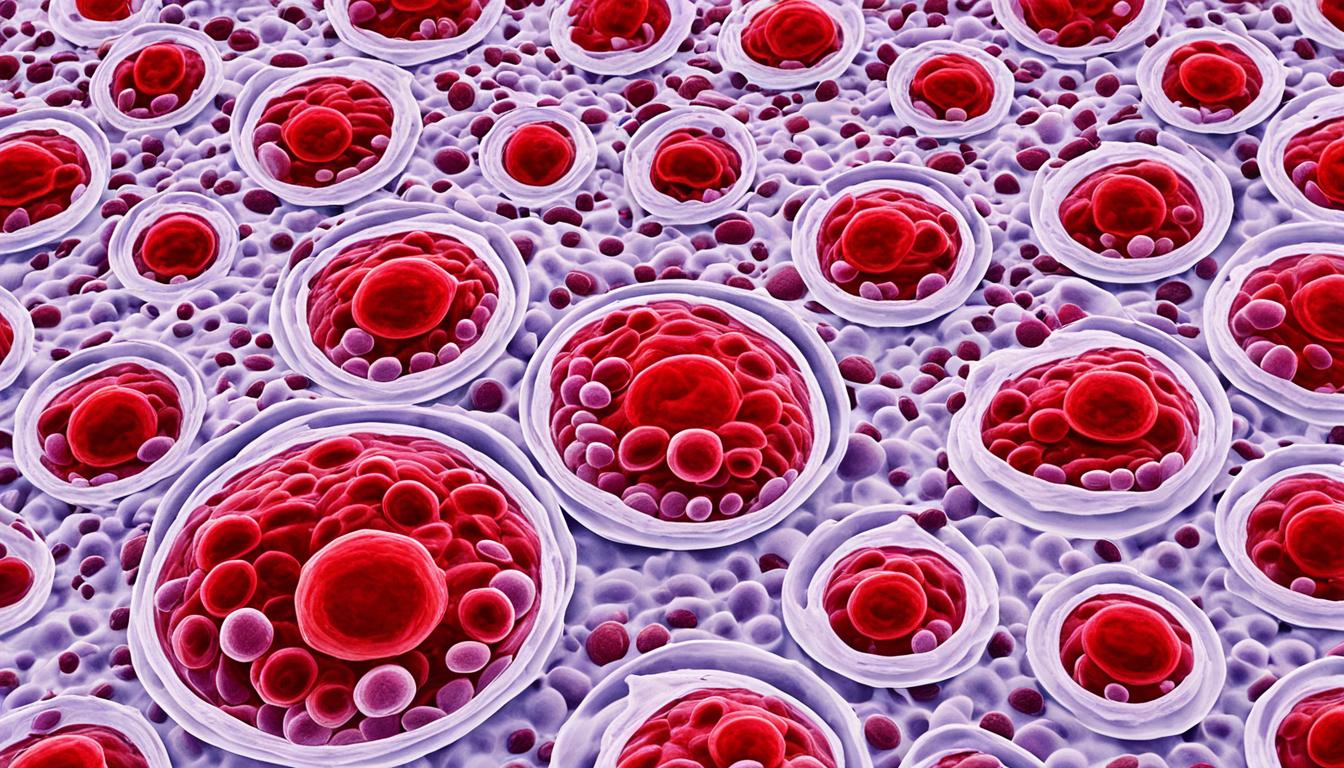
Mediterranean anemia, or beta-thalassemia, is a blood disorder passed down from parents. It affects how hemoglobin in our red blood cells is made. This problem leads to microcytic anemia. This means there are smaller and fewer red blood cells.
People with this condition often feel very tired and weak. They may look pale or have yellowed skin. Some might also have facial bone issues or do not grow quickly. Others show signs like a swollen belly, dark urine, or low appetite. These symptoms happen because the faulty red blood cells carry less oxygen.
This illness is caused by changes in our DNA. These changes affect how hemoglobin’s alpha or beta chains are made. The seriousness of the disease depends on which part of the hemoglobin molecule is changed.
In the Mediterranean, Africa, and Southeast Asia, more people have this illness. This is because these areas see more genetic changes that can cause it.
Treatments aim to make life better for those with Mediterranean anemia. People may need blood from others to get more red blood cells. They might also use chelation therapy to get rid of too much iron. Stem cell or bone marrow transplants could help, along with folic acid to make more blood cells.
Key Takeaways:
- Mediterranean anemia, also known as beta-thalassemia, is an inherited blood disorder affecting hemoglobin production.
- Symptoms of Mediterranean anemia include fatigue, weakness, bone deformities, poor growth, abdominal swelling, and pale or yellowish skin.
- The condition is caused by mutations in the DNA that affect the production of hemoglobin chains.
- Treatment options include blood transfusions, chelation therapy, stem cell or bone marrow transplants, and supplements.
- Mediterranean anemia is more common in individuals of Mediterranean, African, and Southeast Asian descent.
Diagnosing Mediterranean Anemia and Complications
Doctors start diagnosing Mediterranean anemia by checking the patient’s symptoms and history. They use special tests like the Complete Blood Count (CBC) to see if the person has it. This test looks at the levels of different blood cells. In those with the anemia, it often shows low red blood cell and hemoglobin numbers.
Another important test is Hemoglobin Electrophoresis. This test looks at the types and amounts of hemoglobin in the blood. In people with Mediterranean anemia, it shows unusual hemoglobin levels. Then there’s Genetic Testing, which looks for certain genes. It checks if someone has the genes for thalassemia or Mediterranean anemia by studying their DNA for specific changes.
After doctors make the diagnosis, they build a unique treatment plan for each patient. This is based on how bad the anemia is and if there are any other problems.
Complications of Mediterranean Anemia
Mediterranean anemia can cause serious health problems. These can be:
- Iron Overload: People often need blood transfusions. But, too many transfusions can make the body store too much iron. When there’s too much iron, it could hurt organs. Taking medicine to remove the extra iron is important.
- Bone Deformities: Chronic anemia can change how bones grow. This can cause unusual shapes and looks.
- Enlarged Spleen: The spleen gets bigger because it has to clear out bad blood cells. This can lead to belly pain or other issues.
- Slowed Growth Rates: Kids might not grow as fast if their anemia isn’t treated well.
- Heart Problems: The heart might not work as it should. This can lead to serious heart problems.
If anemia causes very bad problems, and usual treatments don’t work, a stem cell or bone marrow transplant might be an option. This aims to use healthy cells to replace the bad ones. It could cure the disease.
| Diagnostic Tests | Key Information |
|---|---|
| Complete Blood Count (CBC) | Measures the levels of red blood cells and hemoglobin. |
| Hemoglobin Electrophoresis | Identifies and quantifies abnormal hemoglobin present in the blood. |
| Genetic Testing | Determines if an individual carries genes for Mediterranean anemia. |
Prevention and Outlook for Mediterranean Anemia
Mediterranean anemia, or beta-thalassemia, is a blood disorder that comes from your parents. You can’t stop getting it, but if you know you carry the genes, you can be smart about family planning. Before starting a family, seeing a genetic counselor is smart. They can help you know the risks.
Doing tests like in vitro fertilization (IVF) with genetic screening can also help. This way, you can pick embryos without the thalassemia gene. This makes it more likely that your child doesn’t have the disease.
The future looks different for people with Mediterranean anemia. It depends on how bad the condition is. But, with the right care, many can live a full, healthy life. Things like blood transfusions or removing extra iron can help a lot.
There’s also hope in new treatments like stem cell therapy. This treatment is showing good signs in helping with the disease. It’s really important for those with Mediterranean anemia to work closely with doctors. Doing what they say can help avoid problems and keep them healthy.