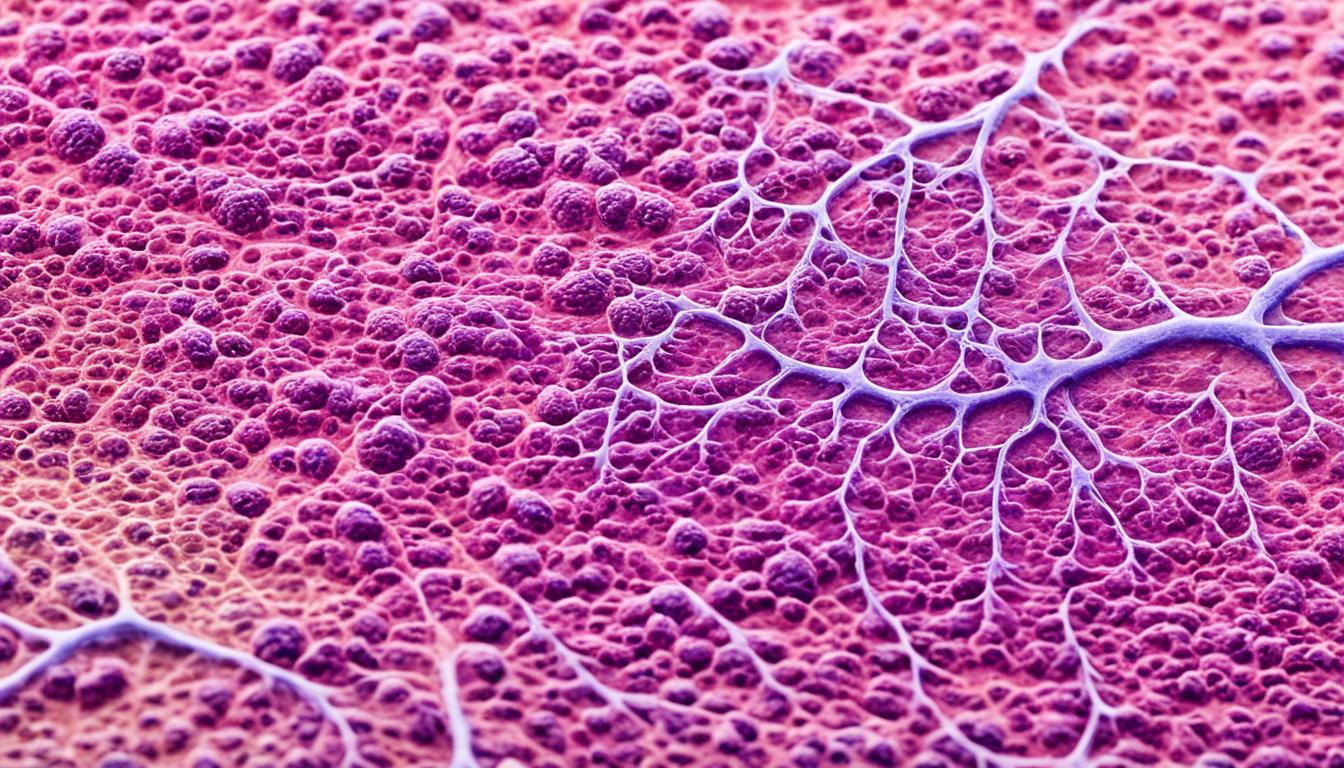
Localized scleroderma is a rare autoimmune disorder. It mainly affects the skin. But, it can also cause issues in other body tissues. This disorder leads to an overproduction of collagen, making the skin thick and fibrous. This can also cause pain and stiffness in the joints.
The usual signs of localized scleroderma are thickened patches or streaks on the skin. These areas might look reddish or purplish and feel tight. They could also limit movement or daily activities in some cases.
There are two types of scleroderma: localized and systemic sclerosis. Localized scleroderma impacts just one area of the body. In contrast, systemic sclerosis can affect various organs. It is important to know that localized scleroderma mostly involves the skin and tissues under it. Yet, systemic sclerosis can harm the lungs, heart, and gut too.
Diagnosing this condition can be hard. Its symptoms can be similar to other skin problems. Health professionals use exams, patient stories, and imaging tests to make a diagnosis. They might also do skin biopsies to look at the tissues closely.
While a cure for localized scleroderma is not yet found, treatments can help manage symptoms. Stem cell therapy, specifically, has had good effects in slowing disease progress and reducing symptoms. This therapy aims to use stem cells to fix and grow back damaged tissues and organs.
Key Takeaways:
- Localized scleroderma is a rare autoimmune disorder characterized by the overproduction of collagen, leading to thickened and fibrous skin.
- Symptoms of localized scleroderma include thickened skin patches or streaks, pain and stiffness in the joints.
- There are two main types of scleroderma: localized and systemic sclerosis.
- Diagnosing localized scleroderma can be challenging, but physical examinations, imaging tests, and biopsies can help.
- While there is no cure for localized scleroderma, stem cell therapy can help manage symptoms and improve quality of life.
Types of Scleroderma
There are two main types of scleroderma: localized and systemic sclerosis. Each has its own set of features and affects the body differently.
Localized Scleroderma
Localized scleroderma impacts a single area, usually the skin. It shows up as thick patches or lines. Unlike systemic sclerosis, it doesn’t affect many organs. This makes it less severe in general.
Systemic Sclerosis
Systemic sclerosis affects both the skin and many organs. It has multiple subtypes that highlight its varied symptoms:
- Diffuse Sclerosis: This subtype involves widespread skin thickening and organ issues.
- Limited Sclerosis (CREST Syndrome): This subtype focuses more on parts of the body, such as the face, hands, and feet. It also includes CREST symptoms.
- Sine Sclerosis: Sine sclerosis features organ damage signs with minor skin changes.
Knowing about these types is key for doctors. It helps them choose the best treatments. Understanding the type and subtype guides medical teams in managing symptoms. This enhances the quality of life for those with scleroderma.
Causes, Diagnosis, and Symptoms of Scleroderma
Scleroderma is thought to be caused by the body’s immune system attacking itself. Its exact cause isn’t known but genetics, chemicals, and changes in the immune system play a role. Hormonal differences might also have an impact.
Diagnosing scleroderma is hard because it shows many symptoms and affects several parts of the body. Doctors use physical exams, blood tests, and biopsies to diagnose it. These tests check the skin’s condition, find specific autoantibodies, and see if any organs are damaged.
Scleroderma often makes the skin thick. It can also cause Raynaud’s phenomenon, where fingers and toes change color and go numb in the cold. Other signs include trouble with digestion, joint pain, fatigue, and problems swallowing.
It doesn’t just affect the skin. Scleroderma can also cause issues with digestion, joints, and severe tiredness. These problems can range from mild discomfort to affecting your everyday life.
Common Symptoms of Scleroderma
| Symptoms | Description |
|---|---|
| Skin Thickening | Involves the thickening and hardening of the skin, mainly on fingers, hands, and face. |
| Raynaud’s Phenomenon | Causes color changes and numbness in fingers and toes when it’s cold or under stress. |
| Digestive Issues | Includes acid reflux & trouble swallowing, leading to more digestive troubles. |
| Joint Pain | Brings pain and stiffness in joints, especially hands and feet. |
| Fatigue | Is extreme tiredness that affects daily life. |
| Difficulty Swallowing | Makes it hard to swallow food or drinks because of esophagus muscle issues. |
Detecting scleroderma early is key to managing it. If you have any symptoms, it’s important to see a doctor. They can do tests for an accurate diagnosis.
Treatment and Management of Scleroderma
Unfortunately, there is no cure for scleroderma. However, many treatments help manage its symptoms and avoid complications.
Medications are key in controlling symptoms such as Raynaud’s phenomenon and thickening skin. They can include drugs that widen blood vessels or ones that lower the immune response. These help ease symptoms and slow the disease’s progress.
Therapies like physical and occupational therapy can improve movement and help keep daily independence. They aim to enhance joint motion, muscle power, and overall body function. This helps those with scleroderma lead an active and satisfying life.
In serious instances, surgery might be required. For example, stem cell transplants have shown great outcomes in regenerating tissues and boosting the immune system. Organ transplants might be needed if the lungs or heart are severely damaged by the disease.
Important changes to daily life can also help manage scleroderma. Being physically active, exercising, and caring for the skin are beneficial. It’s also crucial to avoid cold and stress to keep symptoms under control.
Managing scleroderma can be hard, but there are ways to cope. Being part of a support group and seeking professional advice can offer both mental and emotional support. This can make it easier to deal with the day-to-day and emotional struggles of the disease.
To wrap up, while scleroderma is a lifelong condition with no known cure, a combination of medications, therapies, surgery, lifestyle changes, and support can lead to a better life for those affected.