Leukoplakia is a disorder where white patches appear on the mouth’s lining. It is linked to smoking and drinking. Other causes can be certain infections, constant irritation, and too much sun.
Getting white or gray patches in the mouth is how leukoplakia often shows up. Doctors check by looking and testing, ruling out other reasons for the spots.
Treating leukoplakia depends on how bad it is and if it’s likely to turn cancerous. Options are keeping an eye on it, lifestyle changes, and removing the patches by surgery. People are also looking into using stem cells to treat this condition because stem cells can help repair damaged areas.
Key Takeaways:
- Leukoplakia is a potentially malignant disorder characterized by white patches on the oral mucosa.
- Tobacco smoking and alcohol consumption are common risk factors for leukoplakia.
- Symptoms of leukoplakia include white or grayish patches that cannot be scraped off.
- Diagnosis is made through clinical observation and elimination of other possible causes.
- Treatment options include surveillance, lifestyle changes, and surgical removal of the lesions.
- Stem cell therapy is being studied as a potential treatment for leukoplakia.
Understanding the Pathogenesis and Progression of Leukoplakia
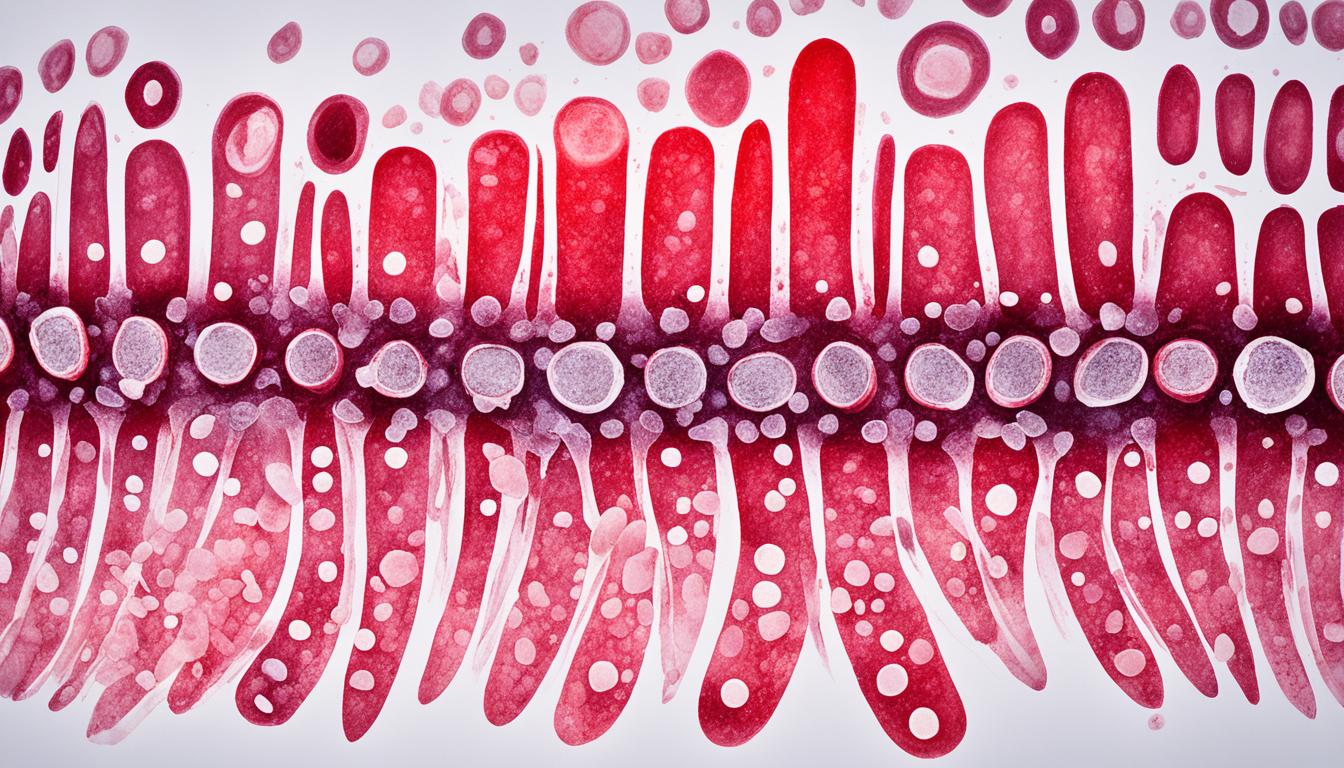
Leukoplakia is a potentially serious disorder in the mouth. It involves both genetic factors and the presence of cancer stem cells. These play a big role in how the disease turns cancerous.
Cancer stem cells are special because they can make more of themselves. They can also change into different cell types. In leukoplakia, these cells might turn into cancer cells. This transformation is important to know about for treating the disease.
During epithelial-mesenchymal transition (EMT), cancer cells can change to become invasive. They lose their old features and gain new ones. This switch helps them spread within the mouth.
Dysplasia shows that leukoplakia cells are changing in a bad way. This bad change increases the risk of getting cancer. Finding and tracking dysplasia early is important for treatment.
There’s a lot of work to find biomarkers for leukoplakia that can show if it might turn cancerous. Biomarkers are signs in the body that a disease is getting worse. Figuring out these signs can help make better treatments and know what to expect for patients.
Understanding leukoplakia helps researchers find ways to target it with therapy. They’re working to make diagnosing it and treating it better. This work aims to help people with leukoplakia have a better outcome.
Key Concepts Related to Leukoplakia Pathogenesis and Progression
| Concept | Description |
|---|---|
| Cancer stem cells | Cells with self-renewal and differentiation abilities implicated in the malignant transformation of leukoplakia. |
| Epithelial-mesenchymal transition (EMT) | A process allowing cancer cells to acquire invasive and migratory capabilities, contributing to leukoplakia progression. |
| Dysplasia | Abnormal cellular changes serving as a precursor to malignancy in leukoplakia. |
| Biomarkers | Molecules or genetic alterations indicating the risk of malignant transformation in leukoplakia and aiding in early detection and prognosis. |
Strategies for the Diagnosis and Treatment of Leukoplakia
To manage and treat leukoplakia, catching it early is key. Early detection means less chance of it turning into cancer. There are important ways to find and treat leukoplakia:
1. Biopsy: The Gold Standard for Diagnosis
If leukoplakia is suspected, a biopsy is vital for diagnosis. A small piece of tissue is taken and checked under a microscope. This check tells us how severe it is and if it might turn into cancer. It is the best way to confirm the presence of leukoplakia and rule out other conditions.
2. Surgical Removal of Leukoplakia
If the growth shows something that could lead to cancer, surgery may be the next step. The aim is to cut out this possible cancer before it becomes a serious problem. Depending on the lesion’s size and position, a variety of surgeries, including laser surgery, can be considered to remove it.
3. Regular Follow-Up and Monitoring
Once a patient has been treated, it’s important to keep an eye on things. Regular visits allow the doctor to see any changes. They’re a way for the doctor to make sure the treatment has worked and that nothing has come back.
Doctors might also order special scans over time to look deeper and check if the disease is spreading. These follow-ups are vital for timely care if something concerning shows up.
4. Lifestyle Changes for Prevention and Management
Changing your lifestyle can help prevent leukoplakia. Stopping smoking and cutting down on alcohol is a big step. Eating well, staying fit, and managing stress are also important. These lifestyle choices can lower your chances of getting leukoplakia again.
Surgical Options for the Treatment of Leukoplakia
| Surgical Option | Advantages | Disadvantages |
|---|---|---|
| Conventional Excision | – Complete removal of lesions | – Risk of post-operative complications – Potential for scarring or functional impairment |
| Carbon Dioxide Laser Excision | – Reduced intraoperative bleeding – Precise and targeted tissue removal – Minimal damage to surrounding tissues |
– Costly equipment and specialized training required – Limited reach in hard-to-reach areas |
| Mucosal Flap Surgery | – Adequate tissue coverage and wound closure | – Complexity and invasiveness of the procedure – Prolonged healing and recovery time |
The surgical type chosen is based on several things. These include where the lesion is, how serious it is, and the patient’s health. Doctors pick the best surgery for each case of leukoplakia carefully.
Conclusion
Leukoplakia is a serious condition in the mouth. It can turn into cancer if not treated early. This disease is part of a group of mouth conditions that might lead to cancer.
It is very important to find and treat leukoplakia early. This can stop it from becoming cancer.
Treatment involves watching the condition, changing your lifestyle, and sometimes surgery. Keeping an eye on it and making positive life changes are important. Doctors also look at using stem cell therapy to repair mouth tissues.
But, we still need more research to fully understand leukoplakia. Scientists want to learn about the genes and other factors that make it happen. This will help improve how we find and treat the disease, which can help patients more.