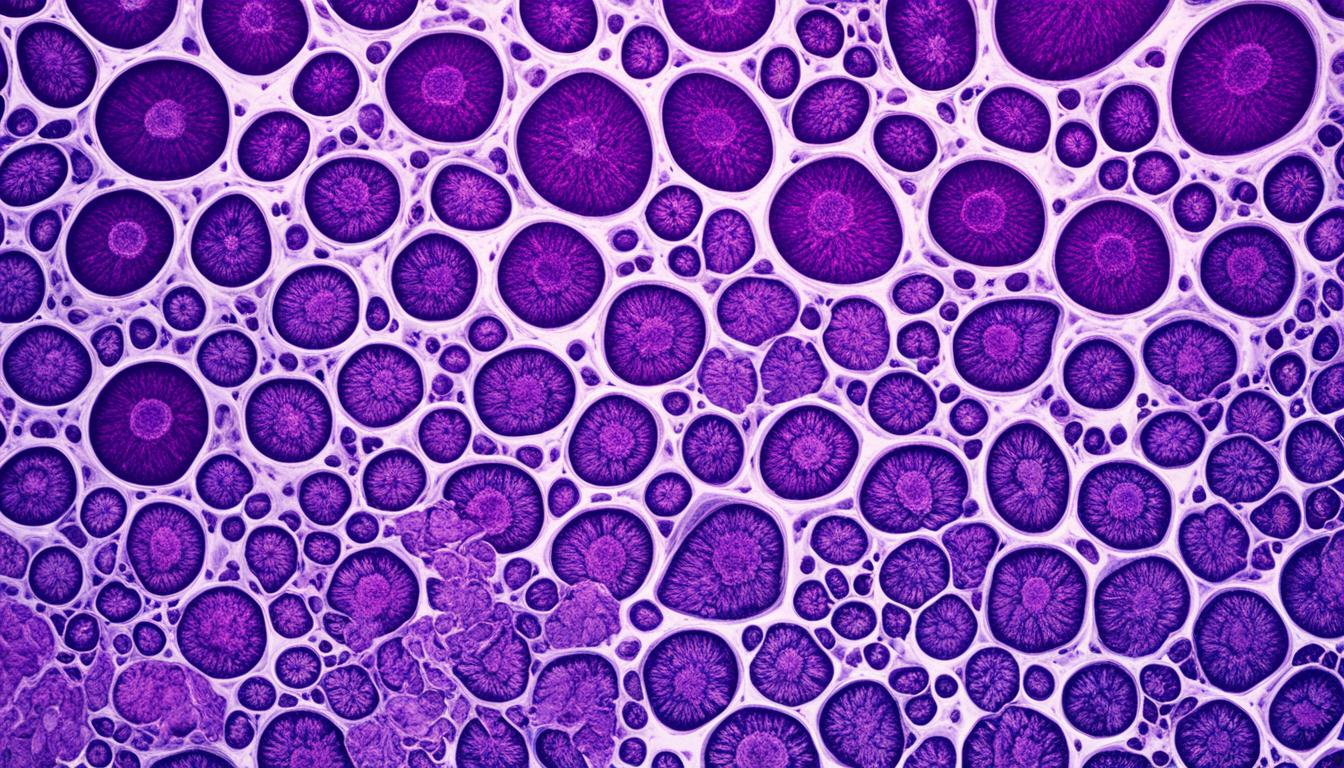
LCIS is a form of noninvasive breast cancer often found by chance during another type of breast test. It shows certain types of cells and changes in the breast’s structure. These signs may also affect the skin around the nipple. A rarer form called pleomorphic LCIS has different cell and tissue features.
LCIS is more likely to appear in both breasts and in more than one location when it does. Over 25 years, about a quarter of people with LCIS might get invasive breast cancer. Treatment can include careful watching, surgery, or using drugs like Nolvadex® to lower the cancer risk. But, necessary to mention, stem cell therapy is not a common treatment for LCIS.
Key Takeaways:
- LCIS is a noninvasive breast cancer condition typically discovered incidentally during a breast biopsy.
- The histologic features of LCIS include the presence of small dyscohesive cells, expanding terminal duct lobular units (TDLUs), and small ducts.
- Pleomorphic LCIS is a variant of LCIS with distinct features.
- LCIS is associated with a higher risk of developing invasive breast cancer.
- Management options for LCIS include observation or prophylactic treatment with anti-estrogens like Nolvadex® to reduce the risk of invasive cancer.
Diagnosis and Risk Factors for LCIS
Diagnosing LCIS often means getting a breast biopsy. This is usually done for other purposes. Doctors look closely at the biopsy under a microscope. They try to find special features that are common in LCIS. Mammograms are done once a year to keep an eye on your breast health, even though they might not show LCIS well.
There are many things that make someone more likely to get LCIS. This includes being before menopause, having family with breast cancer, and having certain genes. Starting your period early and ending menopause later, as well as not having children, can also raise the risk. Using hormones and some lifestyle choices can do the same.
Diagnostic Methods
Doctors often use a breast biopsy to figure out if someone has LCIS. They take out a small bit of breast tissue. Then, they check it under a microscope. This lets them see if the cells look different in a way that suggests LCIS.
Mammograms are x-ray pictures of the breast. They are important for checking your breast health every year, though they may not catch LCIS well. These screening tests are still crucial.
Risk Factors for LCIS
Here are some key risk factors for LCIS:
- Premenopausal Women: Women who haven’t gone through menopause yet are at a higher risk.
- Family History of Breast Cancer: Having close relatives with breast cancer raises your risk.
- Inherited Genetic Predisposition: Mutations in certain genes like BRCA1 and BRCA2 make LCIS more likely.
- Hormone Therapy: Taking hormone-based medicines might increase your risk.
- Early Menarche: Starting your period before 12 years old can also be a risk factor.
- Late Menopause: If you go through menopause after 55, you face a higher risk.
- Nulliparity: Women who never had children have a greater chance of getting LCIS.
| Risk Factors | Description |
|---|---|
| Premenopausal Women | Women who have not yet reached menopause. |
| Family History of Breast Cancer | Individuals with close relatives who have a history of breast cancer. |
| Inherited Genetic Predisposition | Mutations in genes such as BRCA1 and BRCA2. |
| Hormone Therapy | Use of hormone replacement therapy or certain hormone-containing medications. |
| Early Menarche | Onset of menstruation at an early age (before 12 years). |
| Late Menopause | Menopause occurring at a later age (after 55 years). |
| Nulliparity | Women who have never given birth. |
Treatment Options for LCIS
There are many ways to treat lobular carcinoma in situ (LCIS). You can have it removed with surgery. Or, you might take drugs to help prevent it from getting worse. There’s also simply watching and waiting. For some high-risk people, removing the breasts before cancer starts can be an option.
After surgery, many choose to just keep an eye on things, also called observation. This means having regular check-ups and mammograms. The goal is to spot any changes early.
For a different treatment, you might use a drug like Nolvadex® to lower your cancer risk. But, using Nolvadex® can also have its downsides. It might increase your risk of some other health problems. Be sure to talk with your doctor about all of this.
For those at very high risk, removing both breasts before cancer can start is something to think about. But, usually, doctors suggest watching closely or using drugs first. These methods often work pretty well.
In the end, the choice on how to treat LCIS involves your own health details and what you feel comfortable with. Talk this over with your health team. Remember, keeping up with check-ups and tests is key no matter what.
Conclusion
LCIS stands for lobular carcinoma in situ. It’s a noninvasive type of breast cancer. Women with LCIS have a higher risk of getting invasive breast cancer. Doctors often find LCIS by chance during a biopsy for something else. LCIS shows up as a group of small and loose cells.
Treating LCIS offers multiple choices. Some choose surgery, while others go for drugs like Nolvadex®. There’s also the option to just watch and wait. Picking the best treatment is a team effort with your healthcare provider. They’ll look at your risks and what you want.
After choosing a treatment, regular check-ups are a must. These help spot any possible signs of invasive breast cancer early. This way, women with LCIS can work with their doctors to keep their breasts as healthy as possible.