Knee bursitis is a painful issue. It’s about small sacs around the knee getting inflamed. These sacs are filled with fluid and called bursae. Inflammation makes things like walking and climbing stairs hard.
This article looks into knee bursitis symptoms, causes, and how to diagnose it. We’ll talk about various treatments as well. Plus, the potential of using stem cell therapy to help with the pain and swelling.
Key Takeaways:
- Knee bursitis is a condition characterized by inflammation of the bursae around the knee joint.
- Symptoms of knee bursitis include knee pain, swelling, and difficulty with movement.
- The most common causes of knee bursitis are repetitive motions, prolonged pressure on the knee, and certain medical conditions like osteoarthritis or infections.
- Diagnosis of knee bursitis involves a thorough medical history, physical examination, and sometimes imaging tests.
- Treatment options for knee bursitis range from conservative measures, such as rest and medication, to more advanced treatments like corticosteroid injections or surgery.
- Stem cell therapy shows promise in relieving pain and promoting healing in knee bursitis patients.
Types and Causes of Knee Bursitis
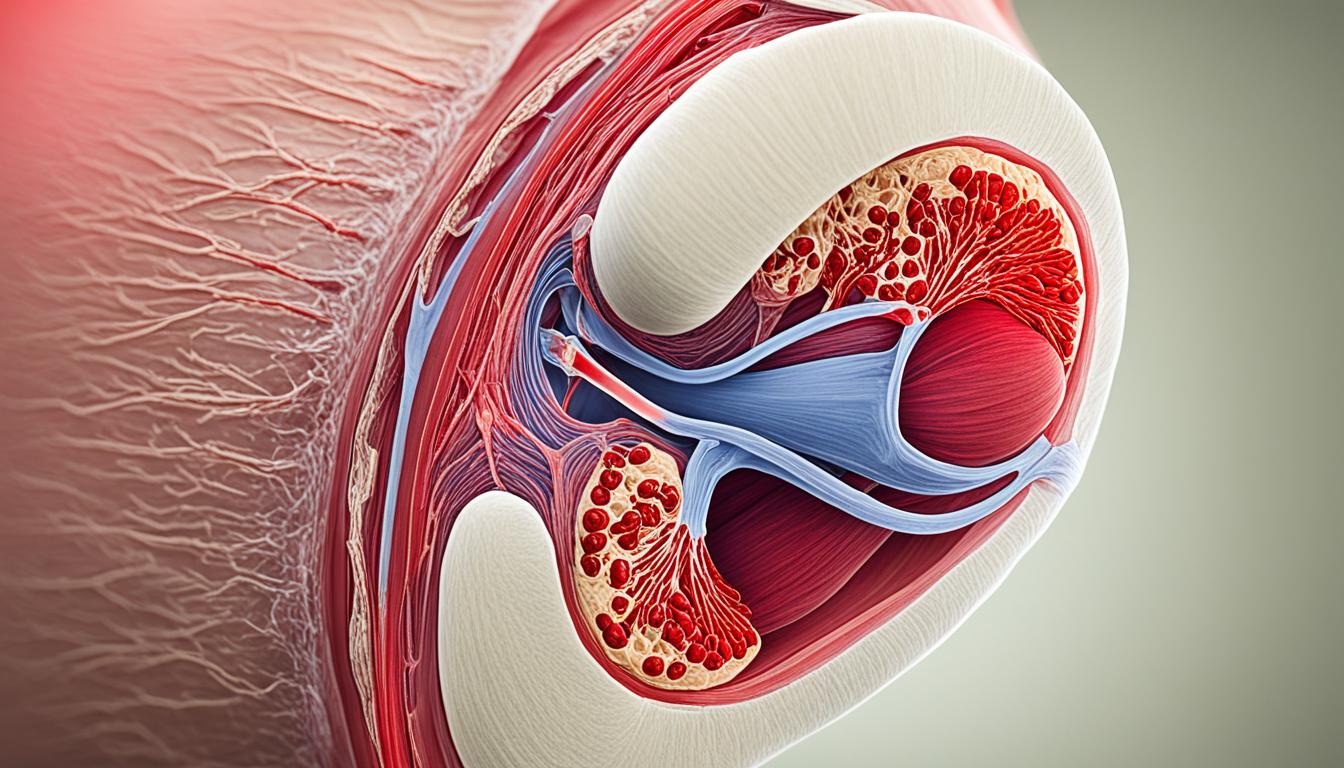
Knee bursitis happens in different places around the knee. This includes the suprapatellar, infrapatellar, prepatellar, and pes anserine bursae. They help reduce friction between tendons, muscles, and bones in the knee, ensuring smooth movement. But, when inflamed, they cause knee bursitis.
Suprapatellar Bursitis
The suprapatellar bursa is right above the kneecap, between thigh muscles and the femur. It can happen because of too much jumping or running. Also, direct hits or infections can cause it.
Infrapatellar Bursitis
The infrapatellar bursa is below the kneecap, between the patellar tendon and the tibia. It’s often linked with activities like gardening or cleaning, which involve a lot of kneeling or crawling. Injuries or infections can also trigger it.
Prepatellar Bursitis
The prepatellar bursa is in front of the kneecap, between the skin and the patella. Known as “housemaid’s knee,” it happens from repeated kneeling or knee trauma. Jobs like carpeting or plumbing, which require a lot of kneeling, can raise its risk.
Pes Anserine Bursitis
The pes anserine bursa is on the inner knee, beneath the joint. Overuse, like from long-distance running or cycling, commonly causes it. Obesity and osteoarthritis also worsen pes anserine bursitis.
Repetitive movements, like jumping, or spending a lot of time on your knees aren’t the only causes. Infections, and diseases like osteoarthritis, rheumatoid arthritis, and gout, can also lead to bursitis. These diseases inflame the joint, causing the bursa to swell.
It’s important to understand the causes to treat knee bursitis effectively. Knowing which bursa is affected and what caused it helps doctors make treatment plans. These plans focus on easing pain, reducing swelling, and speeding up healing.
| Type of Knee Bursitis | Main Causes |
|---|---|
| Suprapatellar Bursitis | Repetitive activities, direct trauma, infections |
| Infrapatellar Bursitis | Excessive kneeling, crawling, injuries, infections |
| Prepatellar Bursitis | Repetitive kneeling, direct trauma |
| Pes Anserine Bursitis | Overuse, repetitive stress, obesity, osteoarthritis |
Symptoms, Diagnosis, and Treatment of Knee Bursitis
Knee bursitis is a painful condition affecting the bursae around the knee. These are small sacs filled with fluid. It’s vital to know the signs, get a proper diagnosis, and find the right treatment to manage this.
Knee Bursitis Symptoms
- Knee pain that worsens with movement
- Tenderness around the affected area
- Redness and swelling in the knee joint
These symptoms can hinder simple activities like walking or sitting for long.
How is Knee Bursitis Diagnosed?
A health expert will ask about your medical history and do a check-up. They’ll press on your knee to see if it’s sore. Sometimes, they’ll use imaging like X-rays to get a closer look.
Treatment Options for Knee Bursitis
There are many ways to treat knee bursitis. This includes simple steps like rest and ice packs to more complex treatments if needed.
| Treatment | Description |
|---|---|
| Rest | Giving the affected knee time to heal by reducing or avoiding activities that exacerbate the pain and inflammation. |
| Ice | Applying ice packs to the knee several times a day to reduce swelling and numb the area. |
| Over-the-counter medication | Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, can help to alleviate pain and reduce inflammation. |
| Physical therapy | Exercises and stretches to strengthen the muscles around the knee, improve flexibility, and promote healing. |
| Corticosteroid injections | Anti-inflammatory medications injected directly into the bursa to relieve pain and reduce inflammation. |
| Surgery | In rare cases when conservative treatments have failed, surgical intervention may be considered to remove the inflamed bursa. |
Treatments vary for each person, depending on how bad the symptoms are. Getting expert advice is key for the right diagnosis and a tailored treatment plan.
Finding Relief and Preventing Knee Bursitis
If you have knee bursitis, you can do several things to ease your pain. First, make sure to rest. This lets your knee start healing. Next, use ice to lower pain and swelling. A compression bandage and elevating your leg will also help with reducing swelling. Taking over-the-counter pain medicine like NSAIDs can also make you feel more comfortable.
Physical therapy is very important for knee bursitis. Therapy aims to make the muscles around your knee stronger. This makes the knee more stable, lowering pressure on the bursa. Your doctor can set you up with exercises that will help you feel better.
Stopping knee bursitis from coming back is the best thing you can do. Keep your weight normal to avoid stressing the knee. Try not to kneel or bend your knee too much. Warm up before any sport or exercise, as this prepares your body for movement.
To stop knee bursitis and prevent it from coming back, follow these tips and get help early. If your knee pain doesn’t go away, see a doctor. They can give you a plan that fits your needs.