Intestinal ischemia is when there is not enough blood flow to the intestines. This can cause tissue damage and serious problems. It’s also called intestinal ischemic syndrome or mesenteric ischemia. It affects how the intestines get oxygen and nutrients and can harm both the big and small intestines.
People with this issue might feel a lot of stomach pain, and even throw up or see blood in their stool. The pain can be very strong and people might feel their stomach is swelling. Because these symptoms are like other stomach problems, getting a correct diagnosis from a doctor is very important.
The reason behind intestinal ischemia can be several things like blood clots or other issues that make blood flow hard. It’s more common in people with heart problems, a past blood clot, or diseases that cause inflammation in the bowels.
Doctors use different tests to see if someone has intestinal ischemia, like CT scans or angiography. They might also check blood for certain signs to make a diagnosis. Finding out about this condition early is key to stopping it from getting worse.
Treatments for this issue depend on a few things like how serious it is or what’s causing it. People might take medicine to break up blood clots or have surgery to fix the blocked blood vessels. There’s also hope in using stem cells to help repair the intestinal tissues. Research is ongoing to explore stem cell therapy’s benefits.
Key Takeaways:
- Intestinal ischemia happens when the intestines don’t get enough blood, leading to harm and serious health risks.
- People might notice strong stomach pain, nausea, and blooding in their stool as symptoms.
- The issue can be linked to blood clots or the narrowing of blood vessels from certain diseases.
- Doctors use advanced tests to spot blockages and find the best way to treat the condition.
- Treatments can range from medicines to surgery, and researchers are looking into how stem cells might aid recovery.
Risk Factors for Intestinal Ischemia
Several factors can raise the risk of having intestinal ischemia. It’s key to know these factors to find those who could be more at risk. By understanding these, doctors can give the right advice and help to lower the risk.
Advanced Age
Getting older is a big risk factor for intestinal ischemia. As people age, their blood vessels might become smaller and less flexible. This makes it hard for blood to get to the intestines, which can cause ischemia.
Underlying Cardiovascular Disease
People with heart issues, high blood pressure, and other cardiovascular diseases face a higher risk. These diseases can lead to atherosclerosis, where arteries narrow. This makes it even harder for blood to reach the intestines.
Smoking
Smoking is a major threat for many diseases, including intestinal ischemia. Cigarette smoke harms blood vessels. This damage can reduce the flow of oxygen and nutrients, causing problems in the intestines.
Obesity
Being obese increases the chance of getting intestinal ischemia. Too much weight makes the heart work harder. This can restrict blood flow and lead to problems.
Diabetes
Diabetes can also up the risk for intestinal ischemia. It can damage blood vessels, which might slow down blood flow to the intestines.
History of Blood Clots
Having had blood clots before, like deep vein thrombosis, can be a sign too. Blood clots can block blood flow. If they reach the intestines, they might cause ischemia.
Inflammatory Bowel Disease and Autoimmune Disorders
Those with conditions like Crohn’s disease and certain autoimmune disorders are also at risk. These conditions can cause inflammation, which might mess up blood flow in the intestines.
If you have these risk factors, taking action to lower your risk is crucial. A healthy lifestyle is key. This means exercising, eating well, and not smoking. It’s also important to manage conditions like high blood pressure and diabetes. If you notice any unusual symptoms, like stomach pain or bowel changes, see a doctor right away. This can help with early detection and treatment.
| Risk Factors | Description |
|---|---|
| Advanced Age | Natural aging can lead to narrower and less flexible blood vessels, increasing the risk of ischemia. |
| Underlying Cardiovascular Disease | Conditions like heart disease and high blood pressure can cause atherosclerosis, narrowing the arteries and restricting blood flow to the intestines. |
| Smoking | Cigarette smoke damages blood vessels, impairing their ability to supply adequate blood flow to the intestines. |
| Obesity | Excess body weight strains the cardiovascular system, reducing blood flow and increasing the risk of ischemia. |
| Diabetes | The complications of diabetes, such as blood vessel damage, contribute to the risk of intestinal ischemia. |
| History of Blood Clots | Prior blood clots can obstruct blood vessels and lead to reduced blood flow and ischemia in the intestines. |
| Inflammatory Bowel Disease and Autoimmune Disorders | Conditions like IBD and certain autoimmune disorders can disrupt blood flow in the intestines, increasing the risk of ischemia. |
Diagnosis and Treatment of Intestinal Ischemia
Doctors usually start diagnosing intestinal ischemia with a physical exam. They also use tests like CT scans, angiography, or ultrasound. These tests help see how blood flows in the intestines. Blood samples can check for signs of damage or infection.
After confirming the diagnosis, a treatment plan is set up. How they treat it depends on how severe it is and its cause.
Doctors might use medicine to break down blood clots or open up blood vessels. This helps improve blood flow and lowers the risk of more damage.
If blocked or narrowed blood vessels are the issue, surgery might be needed. Surgeons could do a thrombectomy to remove clots. Or they might do revascularization to fix blood flow.
Stem cell therapy has shown promise as a newer treatment for this issue. Stem cells can help repair tissue and improve blood flow. Even though it’s still being studied, clinical trials are looking into how well it works for intestinal ischemia.
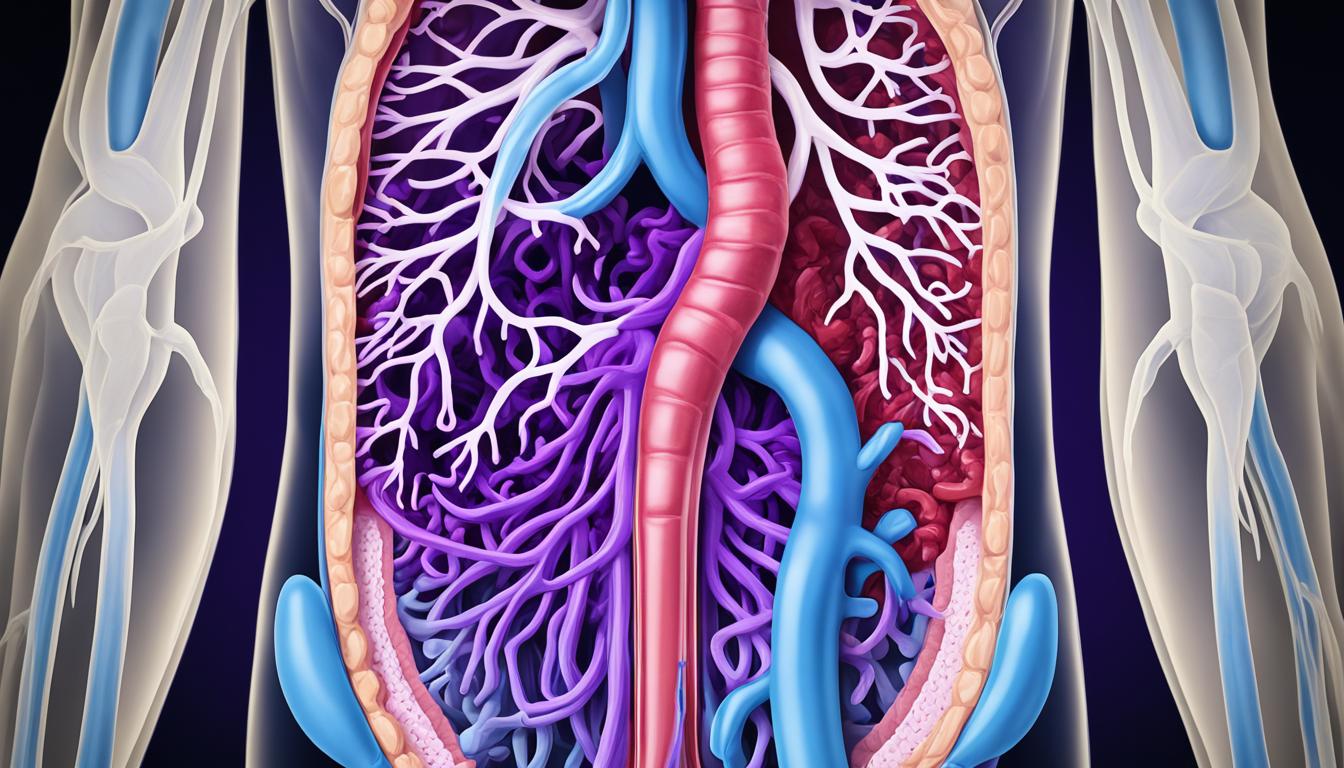
Note: The image above shows how complex the blood vessels in the intestines are. Good blood flow is crucial for the health of your intestines.
Diagnosing and treating intestinal ischemia involves many different specialists. They work together to figure out the best treatments. By catching and treating it early, doctors can help their patients get better and avoid more serious problems.
Conclusion
Intestinal ischemia is a serious issue that demands quick diagnosis and care. Its signs can mimic those of other stomach problems. So, it’s key to see a doctor if you have ongoing belly pain or troubling symptoms.
Alongside common treatments like drugs and surgeries, stem cell therapy shows hope. It could help repair tissues and increase blood flow in people with this condition. Stem cells might fix injured areas and help grow new blood vessels, improving how the gut works and easing symptoms.
But, we need more study to know just how useful stem cell therapy really is for intestinal ischemia. With more trials and scientific progress, stem cell therapy could greatly change how we deal with this disease. The future looks bright, and digging deeper will show us just how much stem cells can help.