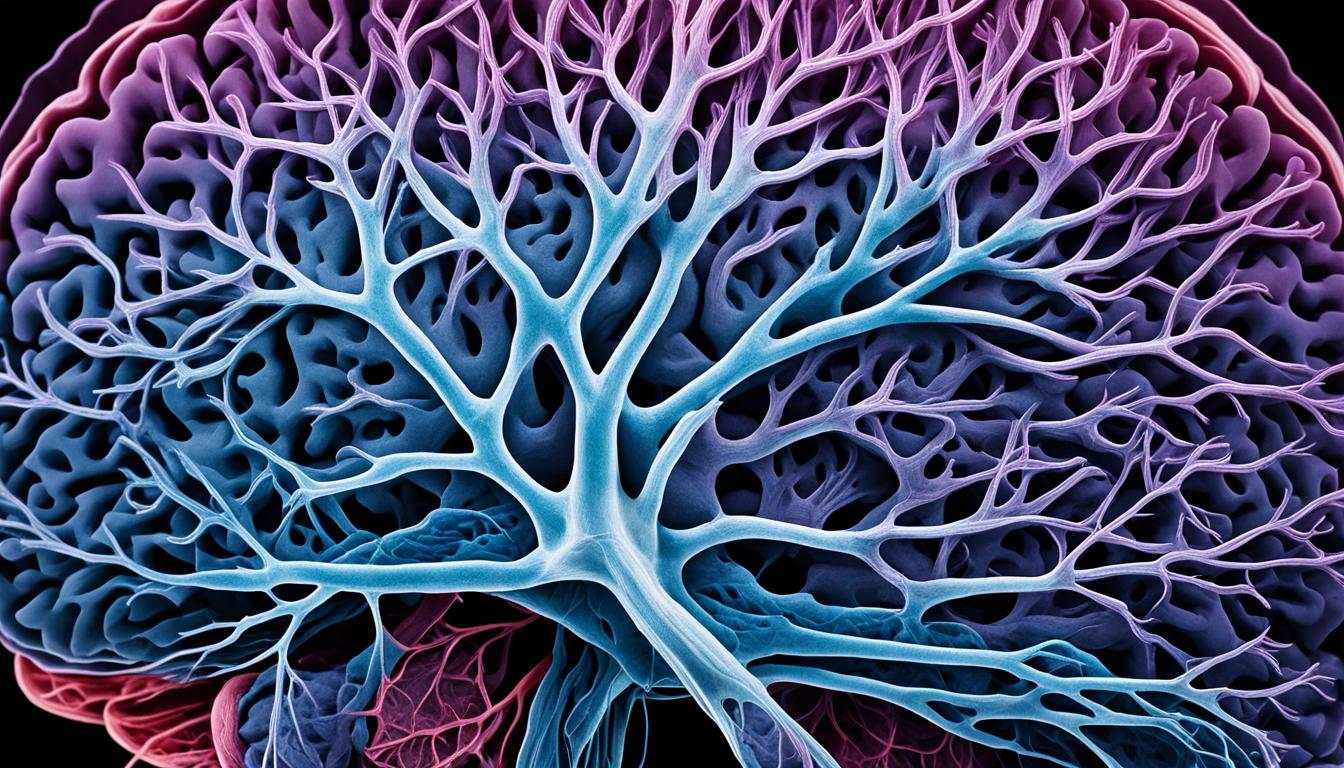
Intracranial venous malformations affect the brain’s blood vessels. They can lead to headaches, seizures, strokes, and brain bleeds. The disease’s severity and how fast it progresses depend on the malformation type.
There are many types, such as AVM, CM, VA, TA, VGM, and MM.
The reason for these malformations isn’t fully known. But, some cases show a link to genes. Scientists are looking into stem cell therapy as a possible treatment.
Key Takeaways:
- Intracranial venous malformations are conditions that affect the blood vessels of the brain.
- Symptoms may include headaches, seizures, strokes, or bleeding in the brain.
- There are several types of intracranial venous malformations, including arteriovenous malformations, cavernous malformations, and venous angiomas.
- The causes of intracranial venous malformations are not fully understood, but a genetic component has been identified in some cases.
- Stem cell therapy is being studied as a potential treatment option for intracranial venous malformations.
Signs and Symptoms of Intracranial Venous Malformations
Intracranial venous malformations show up with various symptoms. These include headaches, seizures, strokes, and cerebral hemorrhage. The type of malformation often determines the specific symptoms.
Arteriovenous Malformations (AVM)
- Progressive enlargement of abnormal arteries and veins in the brain
- Brain cell atrophy
- Hemorrhages
- Seizures
Cavernous Malformations (CM)
- Enlarged collections of blood-filled spaces
- Hemorrhages
- Seizures
Venous Angiomas (VA)
- Enlarged and twisted veins
- Small veins meeting to form part of a larger vein
Telangiectasias (TA)
- Dilation of tiny capillaries
Vein of Galen Malformations (VGM)
- Occurs during fetal development
- Abnormal blood circulation
- Swelling of the brain
Mixed Malformations (MM)
- Combination of arteriovenous malformations and telangiectasias
Severity of these symptoms can differ. They may be unique for each person. Early diagnosis and treatment are key to prevent more issues and help patients.
For a clearer understanding, check out the table below:
| Type of Malformation | Symptoms |
|---|---|
| Arteriovenous Malformations (AVM) | Progressive enlargement of abnormal arteries and veins in the brain, brain cell atrophy, hemorrhages, seizures |
| Cavernous Malformations (CM) | Enlarged collections of blood-filled spaces, hemorrhages, seizures |
| Venous Angiomas (VA) | Enlarged and twisted veins, small veins meeting to form part of a larger vein |
| Telangiectasias (TA) | Dilation of tiny capillaries |
| Vein of Galen Malformations (VGM) | Occurs during fetal development, abnormal blood circulation, swelling of the brain |
| Mixed Malformations (MM) | Combination of arteriovenous malformations and telangiectasias |
The table gives a detailed look at symptoms for each venous malformation type. This helps to understand their characteristics clearly.
Causes and Risk Factors of Intracranial Venous Malformations
The exact causes of intracranial venous malformations aren’t fully known. Evidence shows a genetic link in some. This is especially true for cavernous malformations and telangiectasias.
Genetic diseases come from the genes we inherit from our parents. Sometimes, intracranial venous malformations are from a dominant genetic disorder. Having just one bad gene can mean you get the disease.
With each new baby, there’s a 50% chance they might get the bad gene. But if the disease is recessive, it’s different. Then, you need to get two bad genes to be affected. This makes the chance 25% with each pregnancy.
For X-linked recessive genetic disorders, it’s even more complex. How the disease is passed down changes with the child’s gender. This adds to the challenges of intracranial venous malformations.
| Type of Genetic Disorder | Inheritance Pattern | Risk of Passing on Abnormal Gene |
|---|---|---|
| Dominant Genetic Disorders | Presence of one copy of abnormal gene | 50% with each pregnancy |
| Recessive Genetic Disorders | Inheriting two copies of abnormal gene | 25% with each pregnancy |
| X-linked Recessive Genetic Disorders | Associated with the X chromosome | Different inheritance patterns |
It’s true that some intracranial venous malformations come from genes. But not all cases do. We need more research to understand the full story.
Potential Treatment Options for Intracranial Venous Malformations
Doctors have different ways to treat intracranial venous malformations, which are blood-vessel problems in the brain. The right treatment depends on how severe the issue is. For small malformations that don’t cause harm, doctors might just keep an eye on them. But if the malformation is big or causes problems, treatment is necessary.
One common way to treat these issues is through surgery to remove the malformation. There’s also a method called endovascular embolization, which blocks abnormal blood vessels. Both of these help by fixing the main problem or cutting off its blood supply.
Lately, researchers have been looking at using stem cells to treat these malformations. Stem cell therapy aims to repair damaged blood vessels in the brain. It’s a new approach that looks promising, but we still need more studies to know for sure if it works well and is safe.