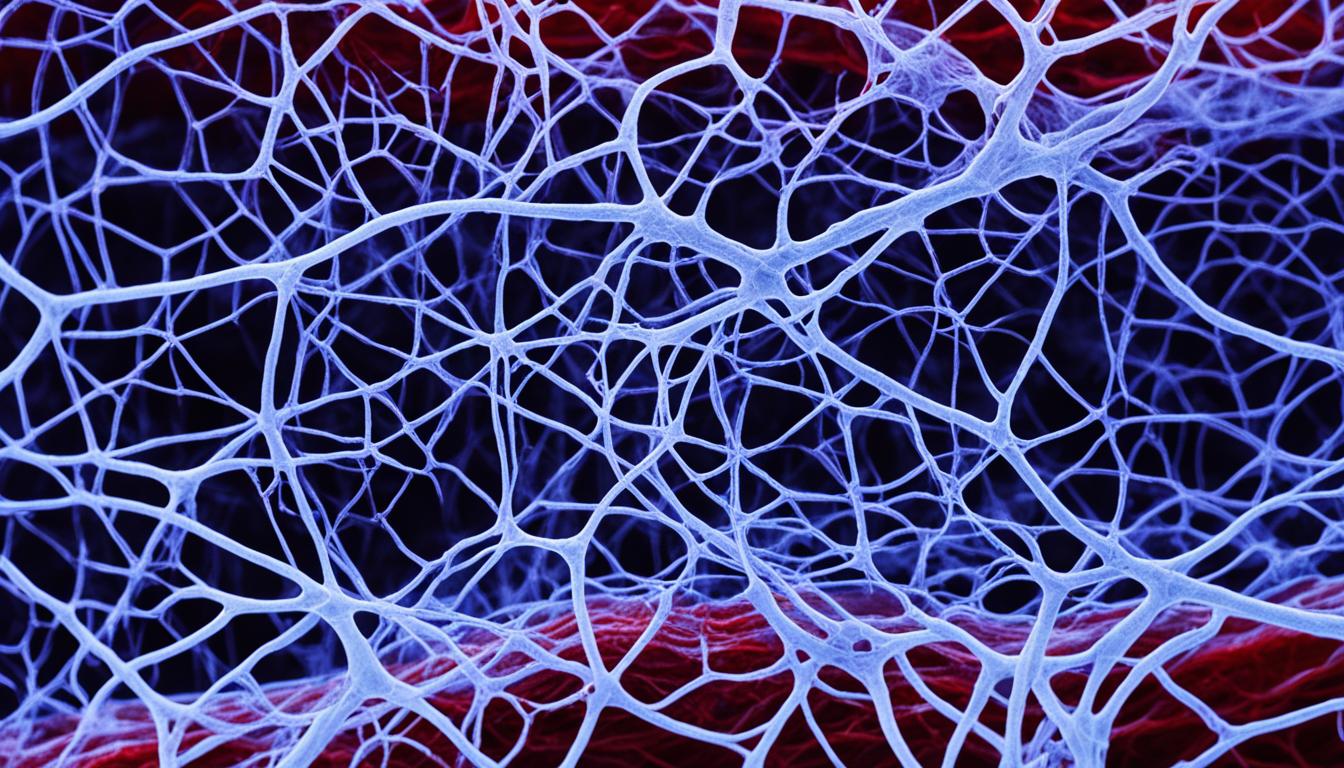
Hereditary hemorrhagic telangiectasia (HHT), or Osler-Weber-Rendu syndrome, is a genetic condition. It causes the growth of abnormal connections between arteries and veins. These connections, known as arteriovenous malformations (AVMs), are often found in the nose, lungs, brain, and liver.
This disorder might lead to serious issues such as bleeding, especially in these areas. It’s important to understand the risks and symptoms of HHT.
Key Takeaways:
- Hereditary hemorrhagic telangiectasia (HHT) is a genetic disorder that causes abnormal connections between arteries and veins.
- AVMs most commonly occur in the nose, lungs, brain, and liver in individuals with HHT.
- HHT can lead to complications such as bleeding and organ rupture.
- Diagnosis of HHT involves physical examination, imaging tests, and genetic testing.
- Stem cell therapy is a promising area of research for potential future treatments for HHT.
Diagnosis and Treatment of Hereditary Hemorrhagic Telangiectasia
Finding out if someone has hereditary hemorrhagic telangiectasia (HHT) requires a close look. Doctors will do a physical exam and ask about your family. They might do imaging tests too. Recognizing HHT early is key to getting the right treatment.
Diagnosis
To diagnose HHT, doctors use special tests to look for AVMs. These can occur in different parts of the body. Tests like Ultrasound can find AVMs in the liver, lungs, and brain.
- Magnetic Resonance Imaging (MRI): MRI creates detailed pictures using magnets and radio waves. It is great for seeing AVMs in important body areas, like the brain.
- Bubble Studies: This test uses gas bubbles and ultrasound to find heart and lung AVMs. Doctors can see how the bubbles move to spot the problem areas.
Genetic testing can tell for sure if you have HHT by looking at specific genes. This is really useful for those with a family history of HHT. It’s also helpful when imaging tests don’t give a clear answer.
Treatment
The aim of treating HHT is to help with symptoms, prevent problems, and enhance life quality. The treatment choice depends on the symptoms, AVM size, and patient health.
Medications: Your doctor might give you medicines to help with HHT symptoms. For low iron levels due to nosebleeds, iron supplements can be used. Other drugs may help with bleeding or prevent organ issues.
Surgical Procedures: Sometimes, surgery is needed for serious AVMs. Doctors can either block off the vessels (embolization) or remove the AVMs.
Lifestyle and Home Remedies: Changes like avoiding certain meds or activities might reduce symptoms. It’s also crucial to see an HHT specialist regularly to check on your condition and treatment.
Complications and Outlook for Individuals with Hereditary Hemorrhagic Telangiectasia
People with Hereditary Hemorrhagic Telangiectasia (HHT) have a high risk of several complications. These come from abnormal connections, or arteriovenous malformations (AVMs), between arteries and veins. Such issues greatly affect the health and outlook for those with HHT.
Iron Deficiency Anemia and its Impact
Iron deficiency anemia is a major issue linked to HHT. Frequent nosebleeds, a common sign of HHT, can cause chronic blood loss. This drops iron levels in the body.
Iron is crucial for making red blood cells. Without enough iron, one might feel tired, weak, or have trouble breathing. Properly dealing with HHT and its nosebleeds is vital in preventing this effect.
Organ Damage and Prognosis
AVMs in organs like the lungs, brain, and liver can cause major problems. Bleeding or breaking of these abnormal connections can damage organs and threaten life. Lung AVMs bring breathlessness, chest pain, and low body oxygen. Brain AVMs can lead to strokes, seizures, or thinking difficulties. Liver AVMs might enlarge the liver, lead to cirrhosis, or heart failure.
The future for individuals with HHT changes based on the AVMs’ severity and location. It also depends on how well treatments work, and the person’s general health. Properly managing HHT, with medical care and treatment, can help people lead full lives.
Life Expectancy and Quality of Life
Life expectancy for those with HHT varies, influenced by condition severity and treatment success. Getting diagnosed early and managing the disease right is key to better outcomes. Improvements in medical care have boosted both life quality and expectancy for these individuals. Still, ongoing medical support and sticking to treatment plans are crucial for the best long-term results.
For those with HHT, getting medical help and following doctor’s advice is a must. Early care, proper treatment, and being alert for possible complications can significantly improve health and outlook for people with HHT.
Advances in Understanding and Treating Hereditary Hemorrhagic Telangiectasia (HHT)
Recent medical research has shined a light on Hereditary Hemorrhagic Telangiectasia (HHT). Scientists and doctors have worked hard to peel back the layers of this genetic disorder.
This journey to understand HHT better has led to big steps forward. One key move is using genetic tests to spot HHT earlier. This helps with quicker treatment and medical care. Doctors now can design treatment plans that fit each patient’s unique genetic makeup.
More exciting news comes from looking at how stem cell therapy could help with HHT. Stem cells have the power to renew and fix problems in blood vessels caused by HHT. Using these new methods, researchers aim to heal damaged blood vessels. This could be a game-changer for people dealing with HHT.
In all, these advances in research and treatments offer real hope for the future of HHT. Even though there’s more to understand, these steps forward are truly promising. They offer a better chance at effective medical solutions for those with this rare disorder.