Hepatic hemangioma (HH) is a common benign liver tumor. It occurs in 0.4% to 7.3% of people. Doctors usually find it by accident during exams. This tumor looks like a large, sealed area. We’re not sure how it forms, but we think it’s due to an issue with blood vessels.
If you have a liver hemangioma, you might feel pain in the upper right side of your stomach. You could also feel full, sick, or have bloating after eating. Large hemangiomas might be really dangerous, causing severe issues like Kasabach-Merrit syndrome or bleeding. Doctors use different tests to confirm if you have this condition.
Usually, small hemangiomas don’t need treatment. But if it causes symptoms or dangerous problems, you might need surgery or other help. Some doctors are even looking at using stem cells to treat these tumors.
Key Takeaways:
- Hepatic hemangioma is the most common benign liver tumor.
- Symptoms may include abdominal pain, discomfort, fullness, nausea, and bloating.
- Giant liver hemangiomas can lead to life-threatening complications.
- Diagnosis is established through various imaging tests.
- Treatment options include surgery, interventions, and stem cell therapy.
Types and Pathophysiology of Liver Hemangioma
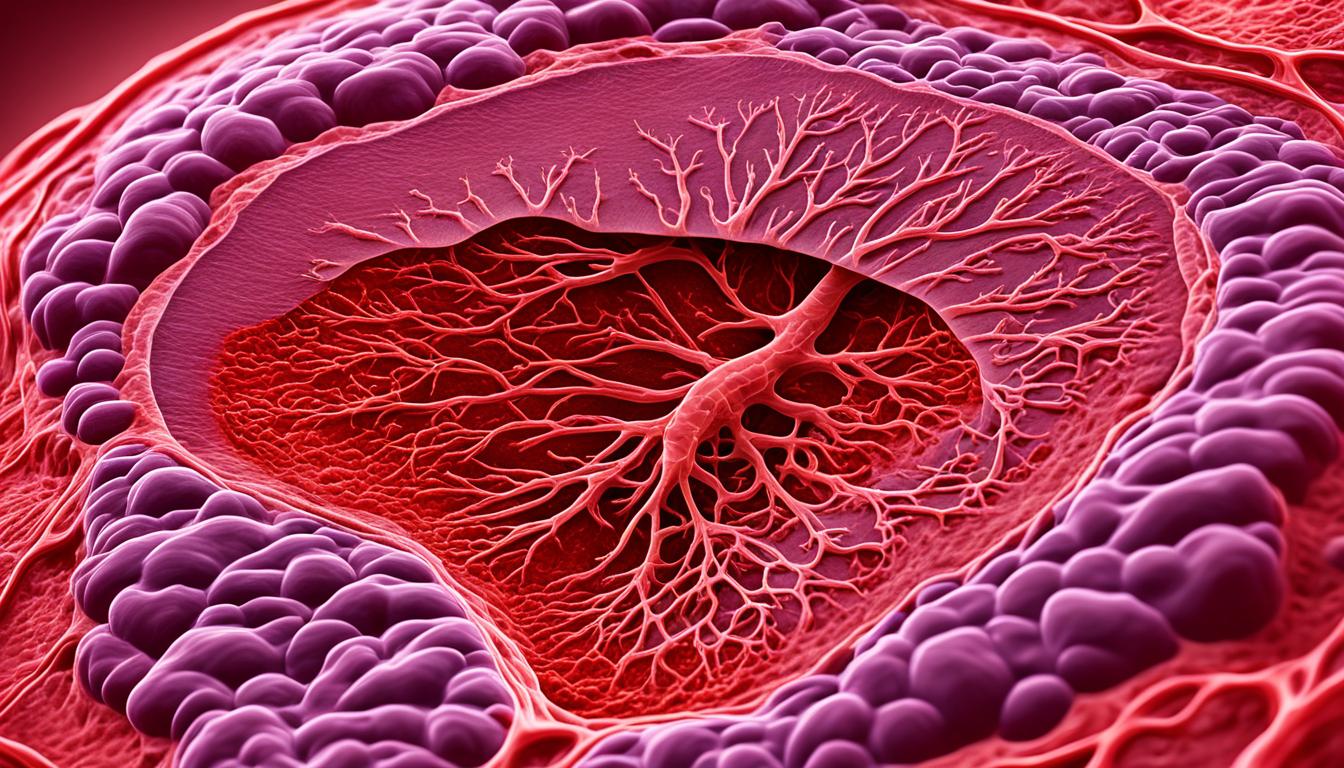
Liver hemangiomas come in three types: cavernous, capillary, and sclerosing. Cavernous hemangiomas are most frequent, featuring large blood-filled spaces. On the other hand, capillary hemangiomas show smaller vessels, and sclerosing hemangiomas involve fiber degeneration.
The exact cause of liver hemangioma development isn’t fully understood. But, experts think it involves unusual blood vessel formation and heightened pro-growth factors. Things like estrogen might affect their size. This is seen in women more, especially when using hormone therapy, birth control pills, and during pregnancy.
Cavernous Hemangioma
Cavernous hemangiomas are common in the liver. They have big blood-filled areas. These spaces vary in size and are covered by endothelial cells.
Usually, they don’t cause major problems. But, if they get too big, they can lead to issues.
Capillary Hemangioma
Capillary hemangiomas in the liver have smaller blood vessels. They form a network of capillaries. These growths are usually harmless. Yet, if they become large, they might cause problems with the liver’s working.
Sclerosing Hemangioma
Sclerosing hemangiomas show fiber degeneration in the liver. They include fibrous tissue and small vessels. These types are not common. Yet, if they get large, they could affect the liver’s function. Generally, they are not cancerous.
Symptoms and Complications of Liver Hemangioma
Liver hemangiomas are often symptomless. But if they grow over 5 cm, symptoms can show up. These include abdominal pain in the right upper quadrant. You may feel discomfort, fullness, nausea, and postprandial bloating.
These issues can impact your daily life and health. In serious cases, liver hemangiomas might cause Kasabach-Merrit syndrome. This is a dangerous condition that involves bleeding problems and can be life-threatening.
Although rare, a liver hemangioma can lead to bleeding due to rupture or trauma. Early medical help is crucial if bleeding signs appear. In some instances, eye issues can also occur.
Common Symptoms and Complications of Liver Hemangioma
| Symptoms | Complications |
|---|---|
| Abdominal pain | Kasabach-Merrit syndrome |
| Discomfort | Bleeding |
| Fullness | Ulceration of the hemangioma |
| Nausea | Ophthalmologic complications |
| Postprandial bloating |
In conclusion, liver hemangiomas might cause abdominal pain, discomfort, and other issues if they get large. Serious complications are rare but can include dangerous syndromes and bleeding. It’s vital to know these risks and get medical help when needed.
Treatment Options for Liver Hemangioma
Small liver hemangiomas that don’t cause symptoms often need no treatment. But if they cause problems, treatment is available.
For larger or troublesome liver hemangiomas, surgery might be the best choice. Doctors can do hepatectomy or liver transplantation. These procedures remove or replace the liver’s affected area. They are effective for long-term control.
Nonsurgical treatments can also help. They aim to stop bleeding or reduce the hemangioma’s size. Arterial embolization cuts off the hemangioma’s blood supply. This causes it to slowly get smaller. Radiofrequency ablation uses heat to destroy the abnormal vessels.
Stem cell therapy is a new and hopeful treatment for liver hemangiomas. Stem cells can turn into different cell types and help in healing. By putting stem cells into the liver, they hope to grow new liver tissue. This could make the hemangioma smaller or less harmful.