Glomerulonephritis is a kidney disease that causes swelling in the small filtering units. They are known as glomeruli. An inflammation in these parts can happen because of infections, autoimmune diseases, or some medications. This disease is a top reason for long-term kidney issues around the world, often leading to kidney damage that cannot be fixed.
The disease shows through swelling, higher blood pressure, odd urine color, and back pain. How bad these symptoms are and their types can change. It starts with an acute phase, usually from infections or the body attacking itself, that can get serious fast. Then, it can turn into a slow-moving, often with lesser symptoms, chronic phase.
Currently, glomerulonephritis is mainly treated with medicines to lower your blood pressure and calm inflammation. But there’s new hope in stem cell therapy. This treatment aims to fix and protect the kidneys in a better way than what’s available now.
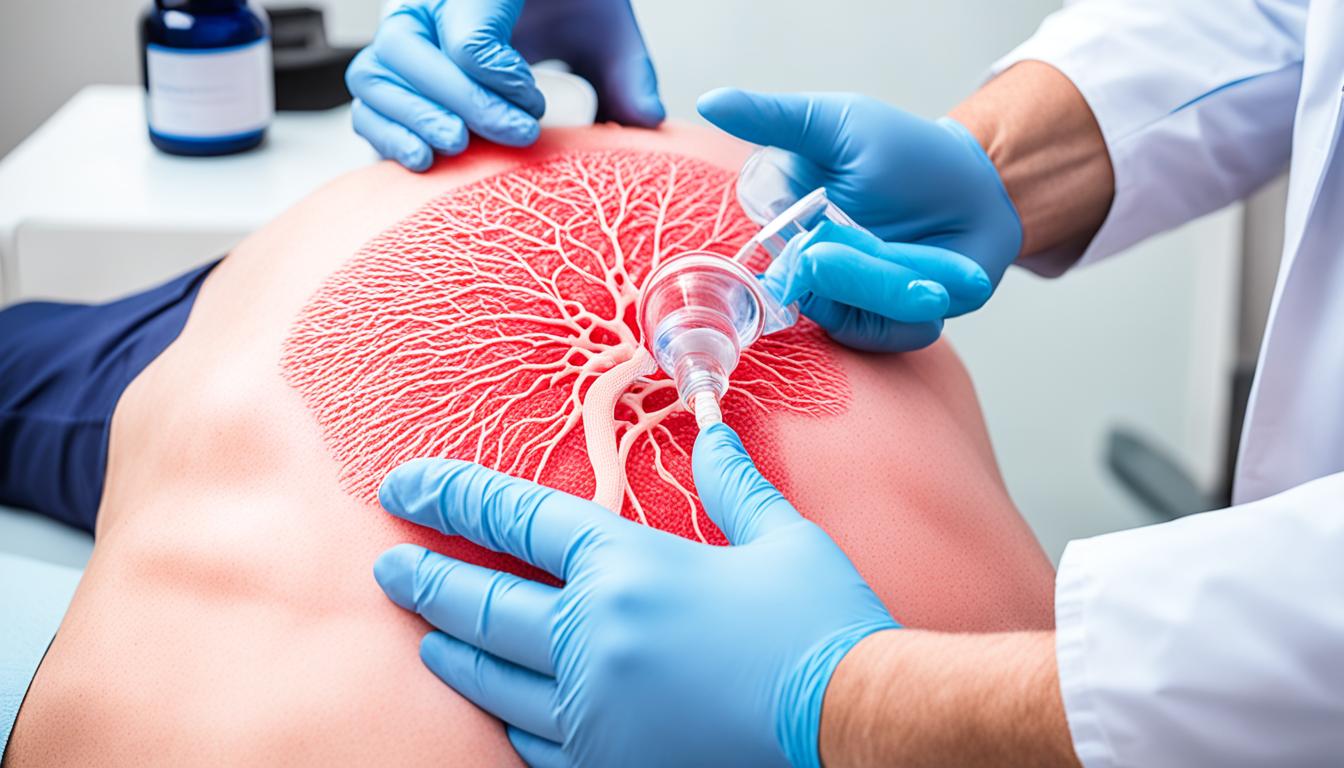
Stem cell therapy uses special cells called mesenchymal stem cells (MSCs). These cells can become many different cell types, including those needed in the kidneys. They could heal the damaged parts of your kidneys. Plus, they help control inflammation and your body’s immune responses, which could save kidneys from further harm.
MSCs were found to stop serious scarring tissue scarring and improve how well kidney cells work. They fight harmful free radicals too, which can harm tissues. Stem cell therapy could be a big change for those whose condition doesn’t get better with current treatments. It offers a chance for a better life quality.
Key Takeaways:
- Glomerulonephritis causes swelling in the kidney’s glomeruli due to inflammation.
- Infections, autoimmune diseases, and some drugs can start it.
- Its signs include swelling, high blood pressure, urine color changes, and back pain.
- While current treatments are there, stem cell therapy is being looked into for better and safer care.
- Mesenchymal stem cells (MSCs) are used in this therapy to support kidney repair.
Types of Glomerulonephritis and Diagnostic Measures
Glomerulonephritis is a serious kidney disease. It shows up as either a sudden problem or a slow one. Each type needs different tests to figure out what’s wrong. Knowing the types and using the right tests is key to helping patients.
Acute Glomerulonephritis
Acute glomerulonephritis comes on fast. It’s often linked to infections or when the body attacks itself. People might see swelling, have high blood pressure, see odd changes in their urine, and feel feverish. Doctors use many tests to check for this type.
- Urinalysis: Doctors check your pee for blood and protein. Finding these things means your kidneys might be hurt or inflamed.
- Blood tests: They also test your blood for creatinine levels. High creatinine shows your kidneys might not be working well.
Chronic Glomerulonephritis
Chronic glomerulonephritis gets worse slowly. People might not notice any signs until it’s well advanced. Finding it early is really hard. Tests look at the kidney’s damage to plan the right care.
- Kidney Biopsy: Doctors may do a biopsy to be sure about the kidney’s damage. They take a small piece of kidney to look at closely.
- Ultrasound Examination: An ultrasound checks the kidneys. It shows their size and shape. This safe test finds any problems in detail.
With these key tests, doctors can pinpoint the type of glomerulonephritis. This helps them give the right care and plan things that suit the patient’s situation.
We’ll talk about how stem cell treatment is showing promise in treating glomerulonephritis next.
Advances in Stem Cell Therapy for Glomerulonephritis
Stem cell therapy is becoming a key player in the fight against glomerulonephritis, a type of kidney disease. It has shown promise in repairing the kidneys. This is largely thanks to mesenchymal stem cells (MSCs) that help replace damaged cells.
MSCs are super useful because they reduce kidney inflammation and suppress the immune system in the kidneys. This is critical in autoimmune glomerulonephritis, where the body mistakenly attacks the kidneys. By keeping inflammation low and immune reactions in check, MSCs help the kidneys heal.
MSCs also stop scarring and boost the health of kidney cells. They fight oxidative stress too, which damages tissues by reducing the number of harmful free radicals. The actions of MSCs on these fronts are key to overall kidney health improvement.
Although stem cell therapy is not the standard for treating glomerulonephritis yet, it’s showing real promise. More study is needed to understand how exactly it works and to make it even better for patients. However, the role of stem cells in repairing and regenerating kidneys gives hope for the disease’s future treatment.