Pulmonary fibrosis is a lung disease that makes the lung tissue thick and scarred. It’s a chronic and steady disease. This condition causes a lot of problems. Patients might feel very short of breath, have a dry cough, or grow thick nails.
The main cause of idiopathic pulmonary fibrosis (IPF) is unclear. People think it might be due to both genes and things in the environment. Those who smoke or are around harmful substances have a higher chance of getting it. So do those with certain viruses or disorders.
Doctors check for pulmonary fibrosis with tests like lung scans and blood exams. Unfortunately, there’s no full cure yet. But, medicines can help slow its progress. In very severe cases, a lung transplant might be the only way to really get rid of it.
Key Takeaways:
- Pulmonary fibrosis hardens and scars the lungs over time.
- It can lead to shortness of breath, a dry cough, and other symptoms.
- The cause of IPF is not completely understood, but genes and the environment play a role.
- Smoking, toxin exposure, and certain illnesses or drugs increase the risk.
- To find out if someone has pulmonary fibrosis, doctors do various tests.
- Medication and lung transplants are the main treatments available today.
- Researchers are looking into stem cell therapy as a potential future treatment.
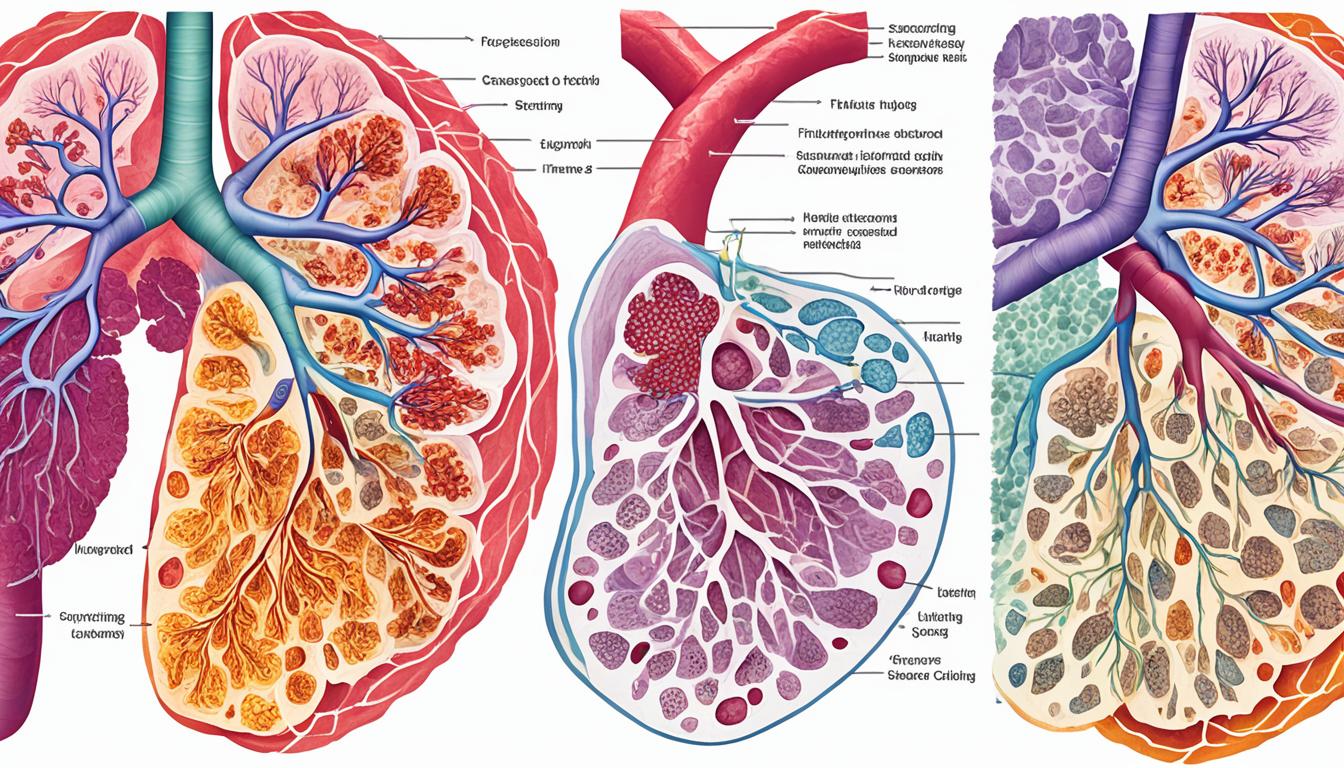
Pathogenesis and Mechanisms of Pulmonary Fibrosis
Pulmonary fibrosis is a disease that causes the lungs to scar and thicken slowly. It’s important to know how this disease starts and works to find good treatments.
Fibroblasts and myofibroblasts are key in making the lung’s tissue thick and scarred. They work by making too many extracellular matrix (ECM) proteins after lung injury. This sets off a cycle of inflammation and scarring.
When lung cells are hurt, they release signals that bring in immune cells. These include macrophages, neutrophils, T cells, and regulatory T cells. These cells either help make the scarring worse or try to stop it, in a kind of fight.
Activating fibroblasts and myofibroblasts make the lung’s tissue layer thicker by putting down more ECM. This thickening makes it hard for the lungs to work right.
Issues with the immune system also make pulmonary fibrosis worse. When immune responses aren’t working as they should, they keep the scarring going.
Fibroblasts and Myofibroblasts
Fibroblasts help heal wounds by making new tissue. They change into myofibroblasts when there’s a wound, and they can pull and make stress on the tissue. This helps fibrosis by making the scarring process stronger.
Inflammation and Immune Dysregulation
Inflammation is a big factor in starting pulmonary fibrosis. It happens when the body sends out signals that bring in immune and healing cells. This also causes more ECM to be made, keeping the scarring going.
Immune problems keep the lung scarring process going. Macrophages, neutrophils, and T cells can help or harm, depending on what they do. Some T cells can stop the scarring, though.
The start of pulmonary fibrosis comes from a mix of many different cells working together. It’s key to understand how these cells interact to find the best treatments.
Current Treatment Options for Pulmonary Fibrosis
Pulmonary fibrosis remains hard to treat, with few choices. Yet, therapies have improved. They aim to slow the disease and make life better for patients.
Medications: Pirfenidone and Nintedanib
Pirfenidone and nintedanib have both got the green light from the FDA for treating IPF. They act by hitting the disease’s underlying causes, cutting down on inflammation and fibrosis in the lungs.
Pirfenidone stops the making of collagen, which is crucial in causing pulmonary fibrosis. It’s proven to slow down the disease and boost lung function in IPF patients.
Nintedanib, a tyrosine kinase inhibitor, goes after various growth factors that spur the fibrotic process. It also slows the disease and lessens lung function decline in IPF patients.
Lung Transplantation
When the disease is too advanced for medicines, lung transplantation might be an option. It can cure the disease by switching out damaged lungs with healthy ones from donors. But, the limited number of available donors and the difficulty of the surgery make this option not widely available.
Stem Cell Therapy
Stem cell therapy is a new hope for pulmonary fibrosis. Stem cells have the power to repair lung damage and control the immune reaction, thanks to their regenerative nature.
Studies show that stem cell therapy can really help with lung fibrosis. Mesenchymal stem cells, especially, can become lung cells and kickstart healing. They can also calm inflammation and stop the fibrosis progress.
Although stem cell therapy is just starting, it’s showing a lot of promise. With more research and technology, it could become a key treatment for this serious disease.
Conclusion
Pulmonary fibrosis research gives hope to those affected by this lung disease. Current treatments are not many, but stem cell therapy shows promise. Scientists have found that stem cells can help the lungs heal and reduce immune reactions.
More studies are required to fully understand how effective stem cell therapy is for pulmonary fibrosis. The field of stem cell technology is advancing fast, bringing new hopes for the future. Ongoing research will help develop better treatments.
Investing in pulmonary fibrosis research could greatly improve patients’ lives. By looking into stem cell therapy and new methods, we aim for a better tomorrow. This effort is vital for those struggling with this disease.