Epididymitis is the inflammation of the epididymis, a tube at the back of the testicle. It stores and moves sperm. It can be short term (acute) or long term (chronic). Pain and swelling behind the testicles are the main signs.
Short term epididymitis is often from sexually transmitted infections. These include Chlamydia trachomatis, Neisseria gonorrhea, and syphilis. Infections not from sex, like Escherichia coli, mostly affect older men. It’s important to detect and treat epididymitis early to avoid problems.
Key Takeaways:
- Epididymitis is the inflammation of the epididymis, which can result in pain and swelling in the testicles.
- Acute epididymitis is often caused by sexually transmitted infections, while non-sexually transmitted infections are more common in older men.
- Prompt diagnosis and appropriate management of epididymitis are crucial to prevent complications and long-term effects.
Epididymis Anatomy and Classification of Epididymitis
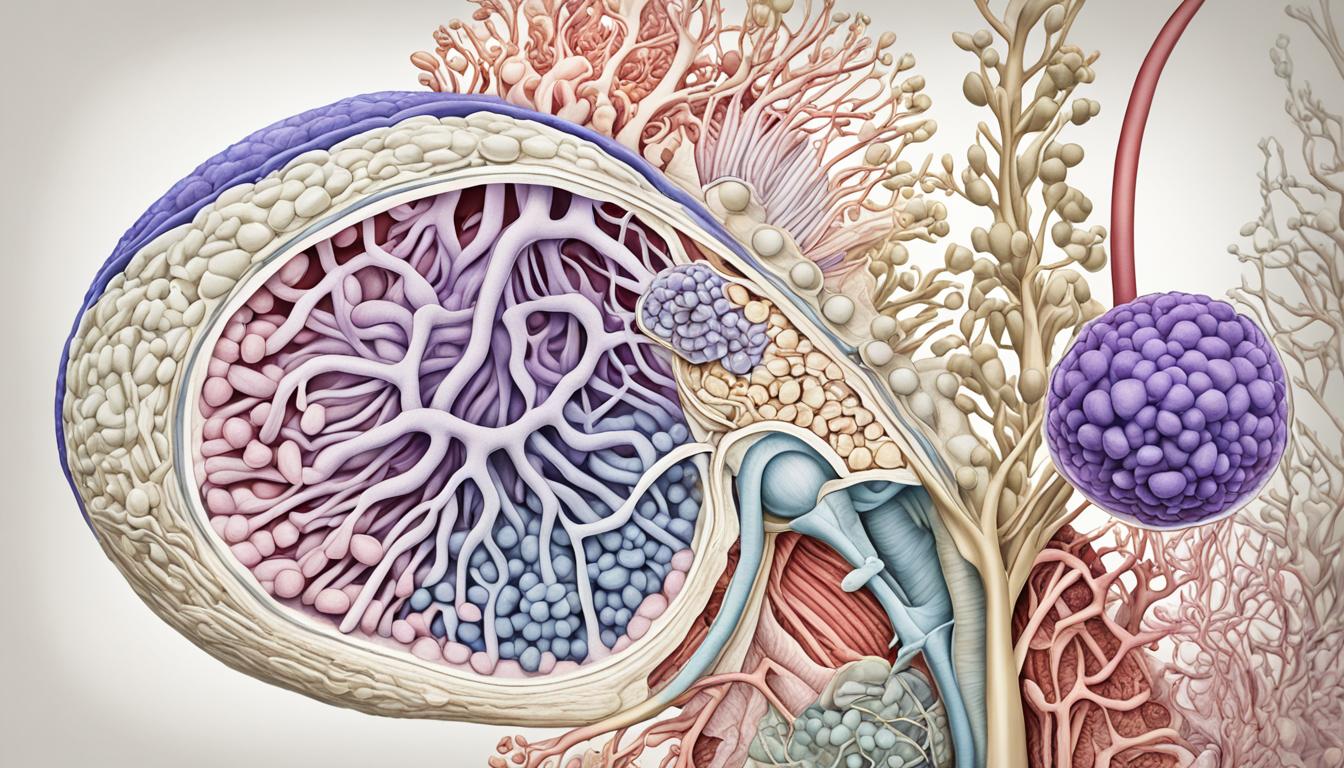
The epididymis is a structure behind the testis. It has three parts: the head, body, and tail. These parts have different roles, with the main job of storing sperm. This process helps sperm mature before leaving the body.
There are two types of epididymitis: acute and chronic. Acute happens quickly over a few days. Chronic epididymitis lasts more than three months. It might be caused by infections or other health issues. Finding these causes is important for the right treatments.
Epididymis Anatomy
This structure plays a key role in the male reproductive system. Found behind each testicle, it works to mature and move sperm. The epididymis has three parts:
| Region | Description |
|---|---|
| Head (Caput Epididymis) | At the top of the testicle, the head collects sperm from the testis. |
| Body (Corpus Epididymis) | The middle part of the epididymis stores and further matures sperm. |
| Tail (Cauda Epididymis) | This part joins the vas deferens, moving mature sperm for ejaculation. |
Classification of Epididymitis
Epididymitis has two types, based on how long symptoms last:
- Acute Epididymitis: It starts suddenly and lasts for a few days. Often, sexually transmitted infections cause this. Quick treatment is important to avoid more serious problems.
- Chronic Epididymitis: This type involves long-term swelling and pain. Many things, from infections to other health issues, could be triggers. Knowing the exact cause helps in planning the best treatments.
Knowing how the epididymis works and about epidemic helps doctors find the right solutions. Next, we’ll talk about what causes epididymitis, who’s at risk, and its symptoms.
Causes, Risk Factors, and Symptoms of Epididymitis
Epididymitis is usually because of an STI. Younger men get it more often. STIs like Chlamydia, Neisseria gonorrhea, and syphilis cause the epididymis to swell.
Other causes are infections of the urinary tract or prostate. So can having a blockage when you pee, or recent surgery. Bacteria like streptococci, staphylococci, and E. coli are often to blame.
Less common causes are viruses (mumps, Coxsackie, varicella zoster) and certain diseases. Some medicines, like amiodarone, may also cause it.
Risk factors include unsafe sex, having a catheter in your urethra, or problems with the bladder emptying. These things make getting epididymitis more likely.
Its symptoms often start with one-sided scrotal pain and swelling. It might hurt when you pee or in your tummy. Sometimes, fever and a strange discharge when you pee happen too.
It’s key to figure out the cause and spot the symptoms early. This leads to better and faster treatment.
| Causes | Risk Factors | Symptoms |
|---|---|---|
|
|
|
Management and Complications of Epididymitis
Epididymitis is treated quickly with proper care. If it comes from a sexual infection, doctors often give azithromycin, ceftriaxone, and doxycycline. For cases not from sex, medicines like ofloxacin are used.
To stop pain, non-steroidal anti-inflammatory drugs (NSAIDs) are recommended. They lower swelling and pain. Also, resting in bed, keeping the scrotum up, and using cold packs help.
If diagnosed, it’s key to finish the treatment and reach out if issues continue. Not treating it well can cause big problems. This includes damaging the testicles, forming abscesses, and blocking the epididymis, which can make someone infertile. Sometimes, when it’s very serious or not going away, removing the epididymis might be needed to stop problems and pain.