Diabetic nephropathy is a type of kidney disease linked with diabetes. People with diabetes are at risk for this condition. It damages the kidneys leading to a gradual function loss.
Its exact causes aren’t fully known. But scientists say it’s due to a mix of genetic, blood flow, and metabolic reasons. It shows up 10-20 years after diabetes starts. Catching it early is key to fight the disease.
Key Takeaways:
- Diabetic nephropathy is a kidney disease associated with diabetes mellitus.
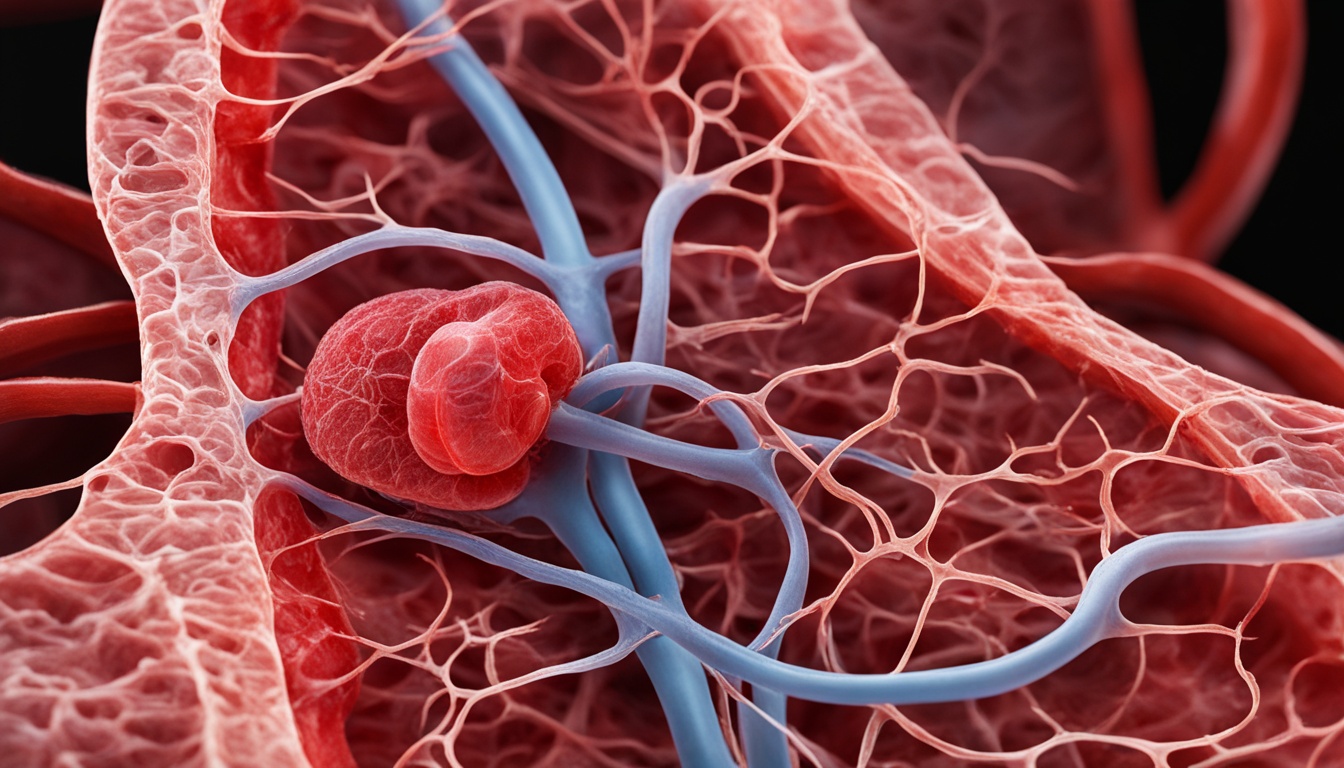
- It is characterized by damage to the renal glomeruli and blood vessels, resulting in a decline in kidney function.
- The exact causes of diabetic nephropathy are not fully understood but are thought to involve genetic, hemodynamic, and metabolic factors.
- Early detection and management of diabetic nephropathy are crucial in slowing the progression of kidney damage.
- Stem cell therapy is emerging as a potential treatment option for diabetic nephropathy, with promising results in early studies.
Treatment options for diabetic nephropathy
Managing diabetic nephropathy involves many treatment options. These aim to control the disease and slow its progress. Treatment focuses on managing diabetes and high blood pressure. These conditions contribute to diabetic nephropathy’s development and worsening.
Lifestyle modifications: Changing habits can greatly help in handling kidney disease. It’s important to keep a healthy weight, exercise regularly, quit smoking, and limit alcohol. A healthy lifestyle can improve kidney function and the person’s health overall.
Dietary changes: A balanced diet is key in diabetic nephropathy care. A doctor may advise a diet low in harmful fats and high in good nutrients. This diet can help manage blood pressure, sugar, and cholesterol.
Prescription medications: Doctors often use medications to treat this condition. They may prescribe drugs to control blood pressure like ACE inhibitors and ARBs. Medicines for blood sugar and cholesterol may also be given.
Invasive Interventions: When kidney disease is severe, other treatments might not work. Then, more aggressive steps might be needed.
- Kidney transplant: End-stage kidney disease may lead to needing a transplant. This could be from a living or deceased donor. A transplant can offer a better life and kidney function.
- Dialysis: For advanced cases, dialysis might be used. It cleans the blood when the kidneys can’t. There are two types, hemodialysis and peritoneal dialysis.
- Stem cell therapy: Stem cell therapy is a new option for nephropathy. It aims to repair kidney tissues using stem cells. It’s still in research but may reverse damage and improve function.
The right treatment for diabetic nephropathy depends on many things. This includes the disease stage, overall health, and what the person prefers. A kidney disease specialist can help make a personalized treatment plan.
Potential future treatments for diabetic nephropathy
Regenerative medicine is paving the way for new treatments for diabetic nephropathy, also known as kidney disease from diabetes. Scientists are looking into new methods like pancreas islet cell transplant and stem cell therapy. These can make life better for those with the disease.
One key method being explored is pancreas islet cell transplant. In this treatment, healthy islet cells from the pancreas are moved into the patient. These cells make insulin, which helps control blood sugar. This move could increase the kidney’s function in patients with diabetic nephropathy.
Stem cell therapy is also a hopeful path. Stem cells can turn into many cell types. In diabetic nephropathy, they might fix damaged kidney tissue. Early trials are showing good results, which gives hope for the future.
These new treatments for diabetic nephropathy are still in the works. But, they bring hope to patients and their families. The possibility of better outcomes and managing this disease more effectively is on the horizon. It could lead to a better future for those living with diabetic nephropathy.