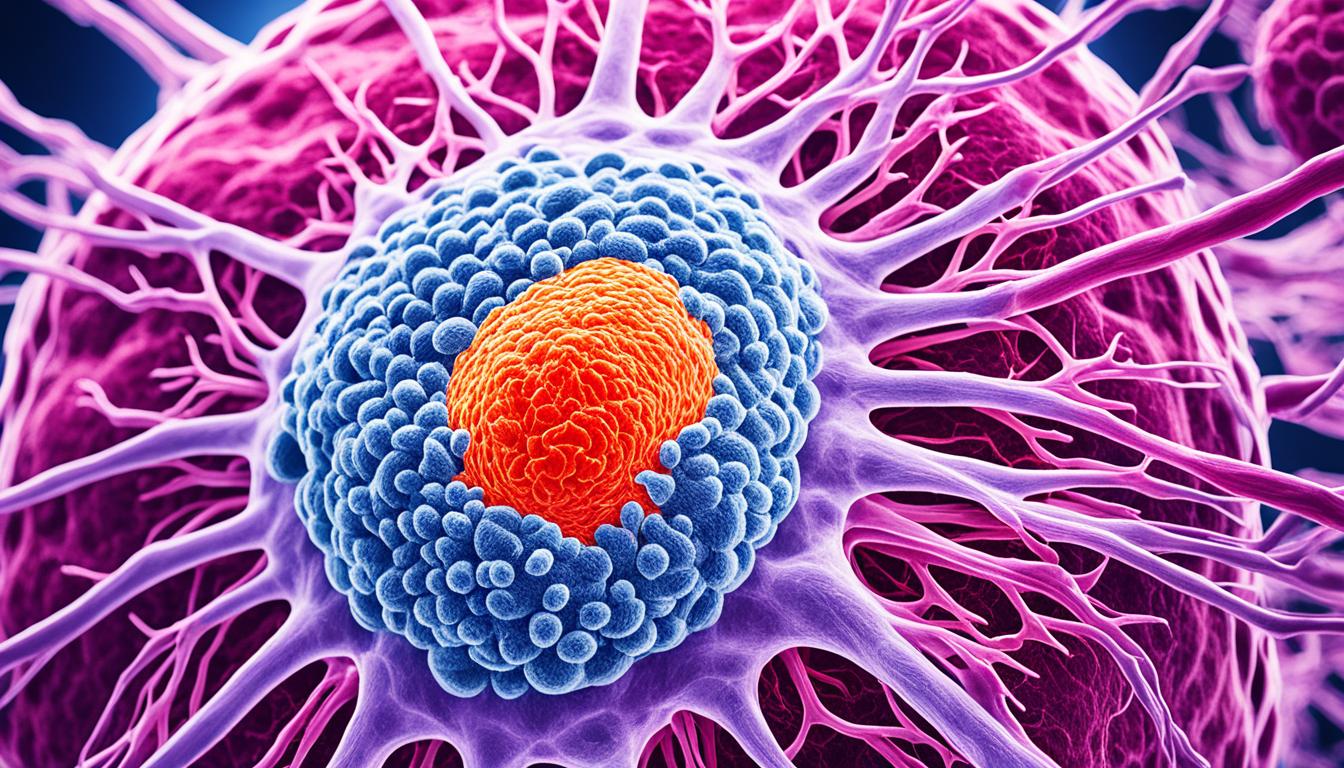
Dermatomyositis is both rare and affects muscle and skin. It affects people of all ages and both males and females. The immune system attacks the body’s blood vessels and skin. This leads to the destruction of muscle tissue. The exact cause isn’t known, but it’s linked to autoimmune diseases.
Those with a weak immune system or a family history of dermatomyositis are at more risk.
The disease shows itself in many ways. You might see muscle weakness, a skin rash, and find it hard to swallow. Other signs include changes in your voice and being tired a lot. Fast recognition of these signs is key for getting quick and right medical help.
To diagnose dermatomyositis, doctors will learn your medical history and do a physical exam. You’ll also have blood tests, an electromyogram, and a magnetic resonance imaging scan. They might also take samples of muscle or skin for further checks. These tests help make sure you have dermatomyositis and not some other condition.
While dermatomyositis has no cure, treatments can help manage its symptoms. You could be given anti-inflammatory or immunosuppressant drugs, or painkillers. Immunoglobulin therapy and surgery for calcium deposits are options too. Physical and speech therapy can also be of great help. Notably, stem cell therapy has shown some great results. It can improve your condition and maybe even turn the disease back.
Key Takeaways:
- Dermatomyositis is a rare inflammatory muscle and skin disease.
- The exact cause of dermatomyositis is unknown but is believed to be related to autoimmune diseases.
- Main symptoms include muscle weakness, skin rash, voice changes, difficulty swallowing, and tiredness.
- Diagnosis involves a thorough medical history, physical examination, and various tests.
- Treatment options include medication, therapy, and stem cell therapy.
Causes and Symptoms of Dermatomyositis
The exact cause of dermatomyositis is a mystery. But, it’s linked to autoimmune diseases. These are diseases where your immune system mistakenly attacks normal, healthy cells. Factors like a weak immune system, a family history of dermatomyositis, and certain illnesses or medications can play a role.
Symptoms of dermatomyositis are noticeable. They include muscle weakness, a distinctive skin rash, and voice changes. You might also face challenges in swallowing and experience muscle tenderness. Other common signs are tiredness, loss of weight, and a fever.
It’s key to spot these signs early and seek help from a doctor. Early diagnosis and treatment are crucial.
Causes of Dermatomyositis
- Weakened immune systems
- Family history of dermatomyositis
- Underlying cancer
- Infectious or toxic agents
- Certain medications
Symptoms of Dermatomyositis
- Muscle weakness
- Skin rash
- Voice changes
- Difficulty swallowing
- Muscle tenderness
- Tiredness
- Unintentional weight loss
- Fever
- Difficulty breathing
- Dry and scaly skin
- Red and swollen fingernail tips
- Formation of calcium deposits under the skin (calcinosis)
Knowing about the causes and symptoms of dermatomyositis is very important. If you show any signs or have potential risk factors, see a doctor. They can perform checks and offer the right care.
Diagnosis and Treatment of Dermatomyositis
To diagnose dermatomyositis, a doctor carefully checks the patient’s past health and does a detailed physical exam. They also do tests to confirm the diagnosis and rule out other diseases. This process is crucial.
Tests might include:
- Blood checks look for signs of muscle inflammation and autoimmune diseases. These help tell dermatomyositis apart from similar illnesses.
- An electromyogram (EMG) finds any strange electrical activity in muscles. This is key for diagnosis.
- MRI scans and chest x-rays can show any inflammation in the body, especially in muscles and lungs.
- Biopsies of muscle or skin are done. Doctors study these samples under a microscope. This confirms dermatomyositis and shows the disease’s severity.
After diagnosing dermatomyositis, the focus turns to {managing symptoms and improving the person’s life. The treatment plan might include several methods:
- A doctor might prescribe anti-inflammatory drugs like corticosteroids. These lessen muscle swelling and ease symptoms.
- Immunosuppressants can be used. They calm the immune system, preventing it from attacking muscles further.
- Pain meds can be given for relief.
- Immunoglobulin therapy might be suggested if other treatments don’t work well. This uses antibodies from healthy donors.
- Surgery is an option for removing painful calcium deposits under the skin.
- Specially designed skin therapies help manage rashes that come with dermatomyositis.
- Physical and speech therapies aid in muscle strengthening and improving function.
Every treatment plan is unique, crafted for the patient’s needs. The plan considers disease severity, general health, and specific goals. It’s very important to stay in regular contact with healthcare providers for treatment updates.
Stem Cell Therapy for Dermatomyositis
Stem cell therapy is a cutting-edge option for treating dermatomyositis. Studies show that stem cells can change the immune system, suppress it, and grow new cells. Stem cell therapy aims to slow down the disease and might even stop it.
The process includes putting stem cells into the patient’s body, either from the patient themselves or a donor. Cells are put in through an IV drip or by injections. The outcomes of this treatment change, depending on the patient’s age, how long they’ve had the disease, and their general health.
This therapy has been successful in many dermatomyositis cases, especially when drugs don’t work anymore. Before starting this treatment, patients must talk about the risks, benefits, and possible side effects with their doctor. Even though the price can change, investing in stem cell therapy might greatly improve the patient’s life.