Degenerative arthritis, known as osteoarthritis, affects many worldwide. Approximately 528 million dealt with it in 2019, and numbers are rising. Aging, obesity, and injuries make people more likely to get it.
The knee, hip, and hand joints are usually hit the hardest. Symptoms include pain, swelling, stiffness, and less joint movement. Cartilage breaks down over time, leading to these issues. Joint injuries or overuse, old age, being overweight, and genetics can raise the risk.
To diagnose, a doctor checks your medical history and does a physical test. X-rays might also be needed. Though there’s no cure, treatments can help, like medicine, therapy, and lifestyle changes. Alternative therapies may also provide relief.
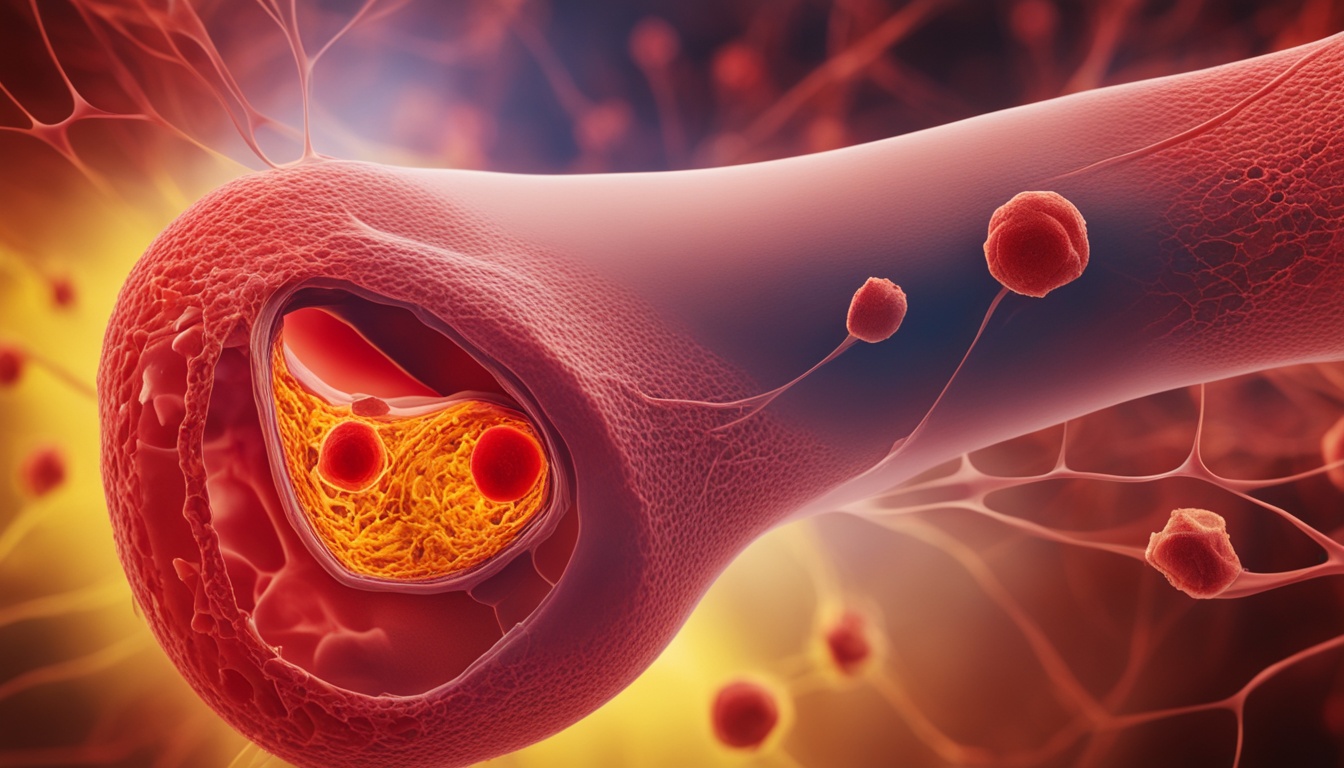
Stem cell therapy is a new area being explored to help with degenerative arthritis. Stem cells can help repair joint tissues, like cartilage. But, it’s still not clear how well this therapy works for this type of arthritis. Many experts do not yet recommend it widely.
Still, there’s a lot of hope for the future of treating degenerative arthritis. Regenerative medicine might bring new ways to understand and deal with this common condition.
Key Takeaways
- Degenerative arthritis, or osteoarthritis, affects millions worldwide, with the knee being the most commonly affected joint.
- Symptoms include pain, swelling, stiffness, and limited range of motion.
- Risk factors include joint injury or overuse, older age, obesity, and specific genetic and metabolic factors.
- Diagnosis involves medical history, physical examination, and imaging studies.
- Treatment options aim to alleviate symptoms and improve joint function, including medication, physical therapy, lifestyle changes, and alternative therapies.
- Stem cell therapy is an exciting area of research, but its efficacy for degenerative arthritis is still under investigation.
- Regenerative medicine offers potential future advancements in the management of degenerative arthritis.
Types of arthritis and their manifestations
Arthritis is a collection of conditions that affect joints and cartilage. The most widespread kinds are osteoarthritis and rheumatoid arthritis.
Osteoarthritis comes from joint cartilage wear and causes pain and stiffness. It usually links to aging and joint stress. The knees, hips, and hands are commonly hit by it.
On the flip side, rheumatoid arthritis is an attack by the immune system on joint linings. It causes ongoing swelling, pain, and stiffness. This ailment can also bring tiredness, fever, and weight loss.
But, arthritis goes beyond just these two types. Here, other kinds stand out:
- Psoriatic arthritis is tied to psoriasis. This skin disease forms red, scaly patches and causes joint issues.
- Gout appears when the body builds up uric acid crystals. It swiftly triggers severe pain, usually in the big toe.
- Lupus arthritis stems from lupus, an autoimmune issue that can harm joints among other parts. It leads to joint ache, stiffness, and swelling.
Lastly, know that arthritis is not the same as arthrosis. Arthrosis refers to age-related joint wear without the inflammation or triggers of an autoimmune disease.
Comparison of Different Types of Arthritis
| Type of Arthritis | Main Symptoms |
|---|---|
| Osteoarthritis | Pain, stiffness, limited range of motion in affected joints |
| Rheumatoid arthritis | Joint pain, inflammation, swelling, fatigue, weight loss |
| Psoriatic arthritis | Joint pain, swelling, stiffness, skin lesions |
| Gout | Intense joint pain, swelling, redness |
| Lupus arthritis | Joint pain, stiffness, swelling, fatigue, skin rashes |
Causes, risk factors, and prevention of degenerative arthritis
The reasons behind degenerative arthritis, also called osteoarthritis, are many. It’s influenced by things like joint injuries, existing joint diseases, and certain metabolic issues such as diabetes. Age and your genes also matter.
Having had joint injuries makes you more likely to get osteoarthritis in later life. These injuries can make joints less stable and damage the cartilage. This makes the joints more prone to wear and tear.
People with rheumatoid arthritis are at higher risk for osteoarthritis too. The ongoing inflammation from rheumatoid arthritis harms the joints over time and affects the cartilage.
Metabolic problems, like diabetes, also up the risk for osteoarthritis. High blood sugar from diabetes is bad for the cartilage. It makes it hard for the cartilage to heal itself.
Being overweight, especially in the hips and knees, is a big factor in osteoarthritis. Extra weight puts more strain on the joints. This speeds up the damage to the cartilage.
As we grow older, our cartilage wears down more easily. Our bodies find it harder to repair the cartilage. This makes getting osteoarthritis more likely as we age.
Some risk factors, like age and genes, are beyond our control. But we can do things to lower the risk of getting osteoarthritis:
- Be careful to avoid joint injuries. Use proper techniques and equipment for physical activities.
- Keep your weight in a healthy range with regular exercise and a good diet.
- If you have diabetes, manage it well. This can help protect your joints.
- Stay active to keep your muscles strong and your joints flexible.
- Don’t strain your joints too much. Make sure to rest after intense activities.
- Use the right shoes and supports like braces to lessen joint stress.
Although we can’t always stop osteoarthritis, we can significantly lower the risk by taking good care of our joints.
Prevention Tips for Degenerative Arthritis:
To prevent or reduce degenerative arthritis, follow these steps:
- Avoid injuring your joints.
- Keep your weight at a healthy level to ease joint strain.
- Control metabolic conditions like diabetes as best as you can.
- Regular exercise helps to keep your joints healthy.
- Don’t put too much pressure on your joints and give them time to recover.
- Use good shoes and supports to protect your joints.
By making these tips a part of your life, you can work toward keeping your joints healthy and lowering your risk of osteoarthritis.
Stem cell therapy for degenerative arthritis and conclusion
Stem cell therapy offers hope for treating degenerative arthritis. These cells can become many types of cells in our body. This offers a way to fix damaged areas, like knee cartilage, and improve how joints work.
Yet, today, stem cell therapy isn’t a top choice for arthritis treatment. This is because there’s not enough solid proof it works well. But, research keeps moving forward. In the years to come, we might see stem cells used more for arthritis.
Degenerative arthritis, also called osteoarthritis, is a big health issue worldwide. We don’t have a full cure. But, we do have ways to manage and lessen its impact on our lives. Stem cell therapy is not a treatment option we often choose yet. However, it opens doors to new possibilities for the future of treating arthritis with regenerative medicine.