Cutaneous T-cell lymphoma (CTCL) is a rare cancer affecting T cells in the skin. This disease causes these white blood cells to behave abnormally. They attack the skin, leading to redness, scaly patches, and tumors. The slow-moving mycosis fungoides and the more severe Sézary syndrome are the main CTCL types.
Treating CTCL involves using skin creams, light, or radiation therapy, and even chemo. It’s key to pinpoint the CTCL type to choose the best treatment. Stem cell therapy is another option in some cases.
Key Takeaways:
- CTCL affects T cells in the skin, making it a unique cancer.
- Symptoms like rash, redness, patches, and tumors mark CTCL.
- The slow mycosis fungoides and the aggressive Sézary syndrome are common.
- Skin creams, lights, chemo, and others are used to treat CTCL.
- Finding the right CTCL type is crucial for the best treatment.
Symptoms and Causes of CTCL
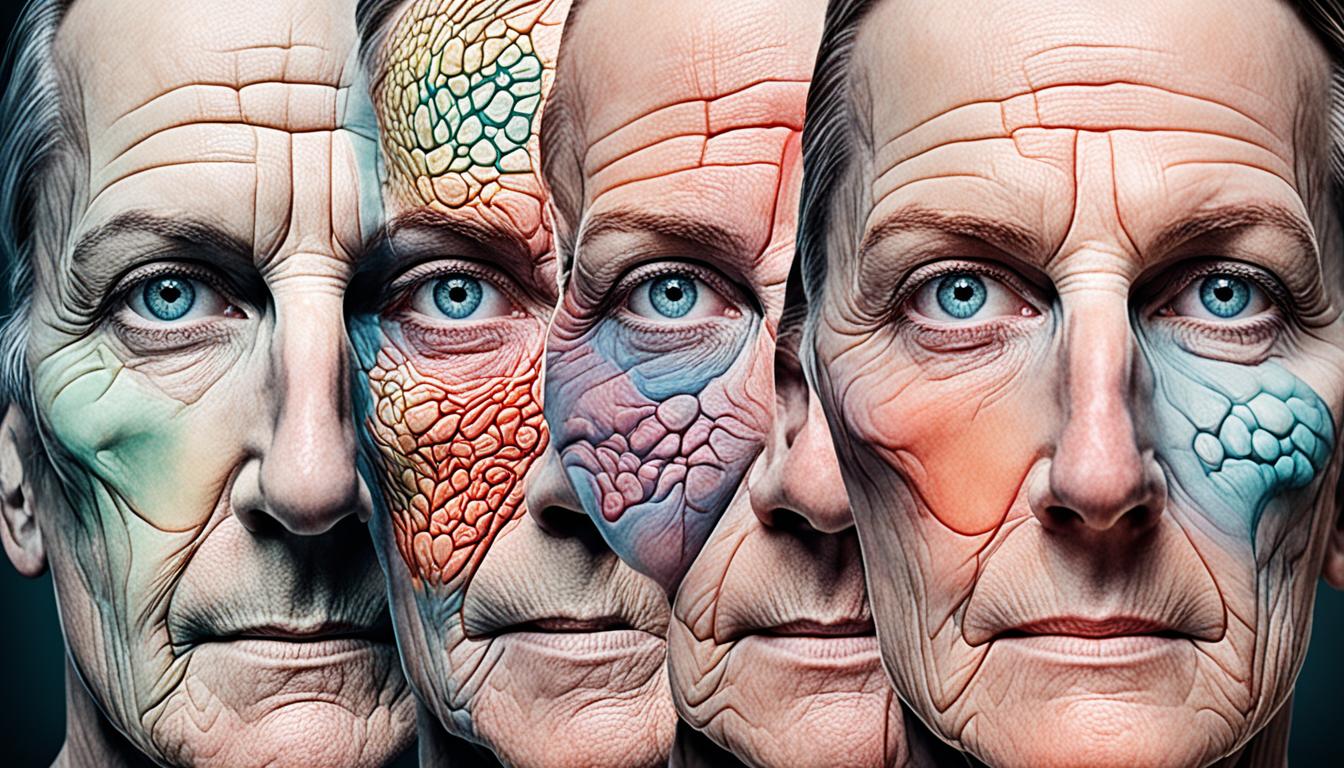
Skin lymphoma, or Cutaneous T-cell lymphoma (CTCL), starts from T cells growing wrong. This causes symptoms like:
- Round patches of itchy, scaly skin
- Patches of lighter skin color
- Skin lumps that may break open
- Enlarged lymph nodes
- Hair loss
- Thickening of the skin on the palms and soles
The symptoms can differ for each person and the kind of CTCL they have. The exact cause isn’t clear, but scientists think gene changes are a big part. These changes make T cells grow the wrong way. Then, these cells can harm the skin, causing CTCL.
Research is working to pinpoint how genes and the world around us may lead to these gene changes. Knowing more about the causes aims to help make treatments that focus on the root issues of the disease.
Types and Impact of CTCL
The term “Cutaneous T-cell lymphoma” covers various subtypes. The most common one is mycosis fungoides. This type grows slowly and mainly affects the skin. It’s important to know that it can spread to lymph nodes and organs in 10% of cases, sometimes causing serious problems.
Sézary syndrome is a more severe subtype of CTCL. It causes a lot of redness on the skin and can spread elsewhere. Even though mycosis fungoides and Sézary syndrome are serious, they usually progress slowly. This makes it possible for people with CTCL to enjoy a good life with the right care.
To manage CTCL well, close monitoring and adjusting treatment plans are key. Working with healthcare experts on a personalized plan can help. This approach allows those with CTCL to control their symptoms and live well.