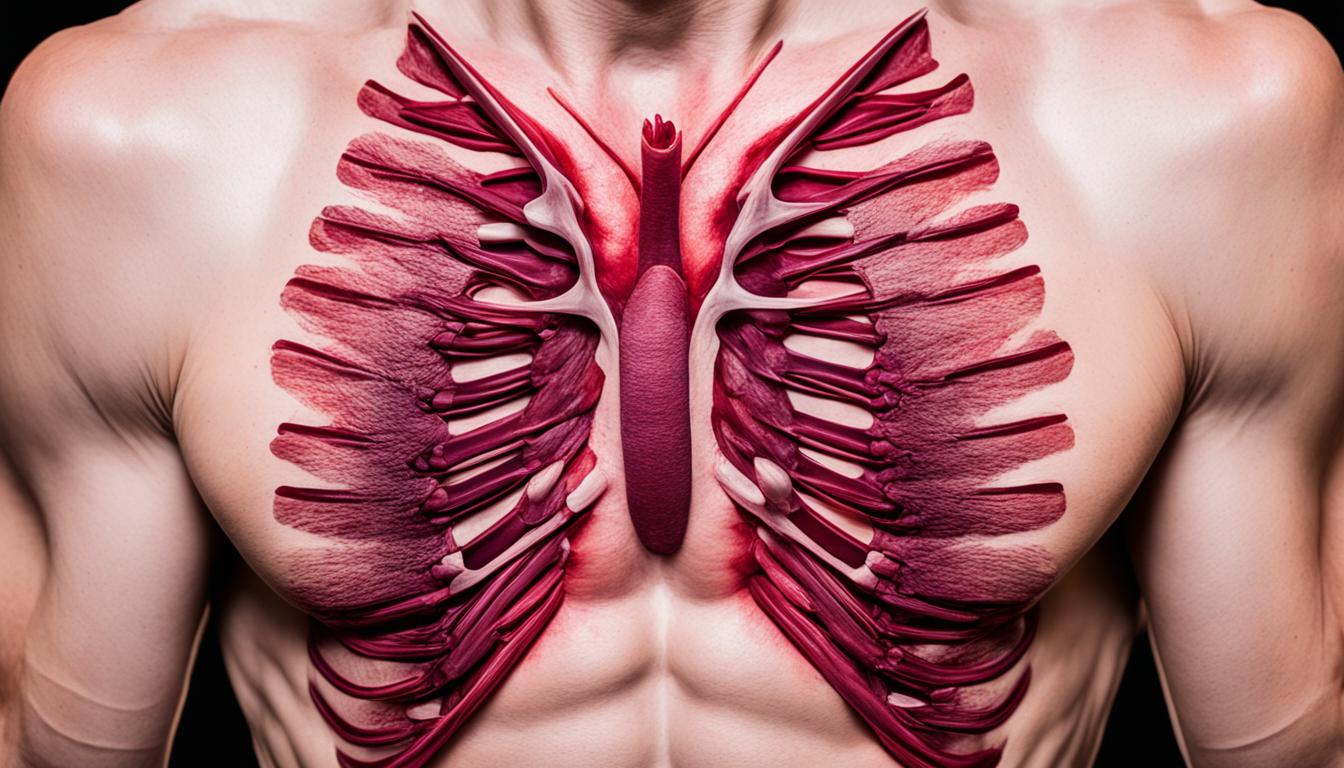
Costochondritis makes the cartilage between a rib and the sternum swell. This leads to sharp chest pain. It can feel like a heart problem. It mainly bothers middle-aged people, especially women. The exact reason it happens is unknown. But, physical strain, viral infections, and certain arthritis types can start it.
Doctors check for costochondritis by first asking about symptoms and past health. They want to make sure it’s not a heart issue or a blood clot. Tests like X-rays and blood tests help them see what’s going on. An electrocardiogram (ECG) is often done too.
Usual care for costochondritis includes resting and taking medications to reduce pain and swelling. But now, stem cell therapy with platelet-rich plasma (PRP) is an option. This treatment aids in healing. It involves injecting the patient’s own platelets into the sore spot.
Key Takeaways:
- Costochondritis is when the cartilage between a rib and the breastbone swells, causing pain.
- It mostly affects those in their midlife, with women more likely to have it.
- Things like overdoing it, catching a bad cold or certain types of arthritis can bring it on.
- Diagnosing it includes looking at the symptoms, health history, and doing tests to rule out other issues.
- Treatments involve resting, taking certain medications, and now, PRP therapy is a promising option.
Symptoms of Costochondritis
The main sign of costochondritis is chest pain. It’s often felt as sharp, stabbing, or aching pain. This pain is usually on one side of the chest. Things like coughing, sneezing, or working hard can make the pain worse. You may feel sore where the ribs meet the sternum, which is called the costochondral joint. In some bad cases, there might be a little mild swelling or inflammation there. When the pain is very strong, you could feel sick.
If you have chest pain, it’s really important to see a doctor. They need to check if there’s something more serious going on. Pain in the chest could have many different causes.
Common symptoms of costochondritis include:
- Sharp, stabbing, or aching pain in the chest
- Pain worsened by chest wall movements (coughing, sneezing, exertion)
- Tenderness at the junction of the ribs and sternum
- Mild swelling or inflammation of the costochondral cartilage or joints
- Nausea (in severe cases)
Causes and Diagnosis of Costochondritis
Costochondritis makes the cartilage from a rib to the sternum inflamed, causing chest wall pain. Its exact cause is usually a mystery, but it has connections to several things.
One probable cause is chest wall injuries from falls, accidents, or direct hits. Tasks that require a lot of arm and upper body use over time can also play a part.
Infections like the common cold or flu can start off costochondritis. They cause the chest wall to get inflamed, leading to pain and soreness.
Arthritis types like rheumatoid arthritis and ankylosing spondylitis might increase costochondritis risk. These conditions make the body attack its own joints and tissues, including chest wall cartilage.
Even bacterial infections can sometimes be behind costochondritis. Bacteria, for example Staphylococcus aureus, can cause chest wall cartilage and nearby tissues to get inflamed and pained.
To diagnose this, a doctor will do a careful physical exam. They check for tenderness, swelling, and ask about your recent health history and activities.
They must also make sure it’s not a more serious issue like a heart attack. This could require tests such as blood tests, X-rays, and an ECG to examine the heart’s rhythms.
Imaging tests like CT scans or MRIs might help more clearly see chest wall inflammation. These can also rule out other sources of chest pain.
Finding the true cause of costochondritis is key to healing. This knowledge helps doctors plan the right treatment for those with chest pain.
Stem Cell Therapy for Costochondritis
Platelet-rich plasma (PRP) therapy is showing great promise in treating chest wall pain from costochondritis. This method involves taking blood from the patient, separating out the platelets, and injecting the concentrated mix into the area that needs healing. The PRP has a lot of growth factors that help the body heal and reduce pain.
The key to PRP’s success in treating costochondritis is in the number of platelets used. More platelets often lead to better results. That’s why it’s best to go to a clinic that can tailor the PRP mix for your specific needs, using the latest technology.
Aside from PRP, other ways to treat costochondritis include rest, taking NSAIDs, and using ice or heat on the sore area. It’s very important to see a doctor to get the right diagnosis and treatment plan. They’ll be able to suggest what’s best for you.