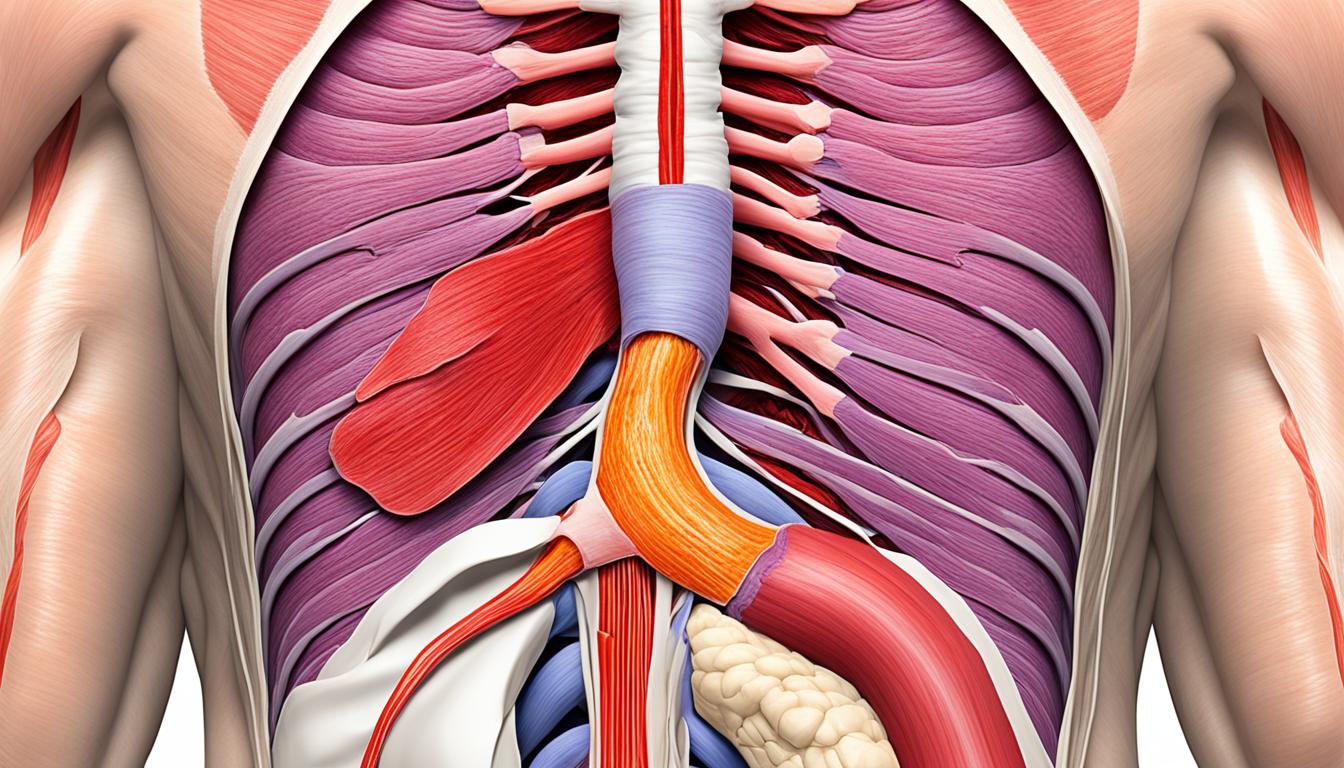
Cardiospasm, also called achalasia, is a rare issue with how the esophagus works. It happens when the lower esophageal sphincter doesn’t relax properly after you swallow. This makes it hard for food to move from your esophagus to your stomach.
Its key signs are trouble when you’re swallowing, a feeling of fullness under your chest, throwing up food, and losing weight. Doctors might think it’s another condition like heartburn or a hiatal hernia at first. To confirm, they use a test called high-resolution manometry. This test checks the LES and the way your esophagus moves.
Stem cell therapy is showing a lot of hope in helping those with cardiospasm. It aims to improve the movement of the esophagus.
Key Takeaways:
- Cardiospasm is an esophageal motility disorder characterized by the loss of inhibitory neuronal function in the esophagus.
- Symptoms of cardiospasm include difficulty swallowing, substernal discomfort, food regurgitation, and weight loss.
- Diagnosis is primarily done through high-resolution manometry, which shows abnormal LES relaxation and a non-peristaltic esophageal body.
- Stem cell therapy shows promise in restoring esophageal motility in patients with cardiospasm.
- Further research and clinical trials are needed to fully understand the efficacy and long-term effects of stem cell therapy in treating cardiospasm.
Causes of Cardiospasm
The cause of cardiospasm isn’t fully understood, but experts think many factors play a part. They believe a virus and genetics could mix to spark an immune reaction in the esophagus’s nerves. This can damage the nerves and cause problems like aperistalsis and LES not relaxing.
These nerve issues lead to typical cardiospasm symptoms. For example, the esophagus can’t move food down properly, and the LES doesn’t open as it should. Inflammation is key here, as it disturbs how the esophagus works.
Also, things in the environment might add to different cardiospasm types. These, with the body’s immune reaction, may lead to problems in controlling how the esophagus muscles work. Some may lose their ability to restrict, while others might have too much excitement or inhibition.
Viral Infection and Genetic Predisposition
A virus starts off by inflaming the esophagus’s nerves and ganglia. This, along with a genetic leaning, disrupts regular esophagus function. It starts the cardiospasm development process.
Environmental Triggers and Neuronal Damage
External triggers, such as harmful substances, can worsen the inflammatory response. They can also damage the esophagus’s nerves. This damage can mess with the LES’s function, brings about cardiospasm symptoms.
Inflammation and Esophageal Dysfunction
Inflammation is a big part in making cardiospasm happen. After a virus and due to things in the environment, the immune system keeps sending signals that lead to the esophagus being inflamed. This can damage the nerves and muscles of the esophagus.
Due to this inflammation, swallowing gets hard, and the LES doesn’t open right, lowering the person’s life quality. Knowing what causes cardiospasm is key to treat it better. The goal is to repair how the esophagus works and help patients feel better.
Diagnosis of Cardiospasm
Finding out someone has cardiospasm is very important. It helps doctors treat the issue correctly. To diagnose it, several tests are used. They also check if there are other problems in the esophagus. The main test is called high-resolution manometry. This test looks closely at the esophagus, especially at a part called the lower esophageal sphincter.
In high-resolution manometry, a doctor puts a thin tube with special sensors into your throat. You drink water or a special liquid with this tube in your throat. This makes the muscles in your esophagus move. The sensors check these muscle movements. If your lower esophageal sphincter doesn’t relax like it should after you swallow, it could mean you have cardiospasm.
Doctors might do more tests besides high-resolution manometry. One common test is a barium swallow. You drink a liquid with barium in it. Then, the doctor takes pictures of your esophagus using X-rays. The barium makes your esophagus show up clearly. It helps doctors see if your esophagus is the right size and shape. They can also look for any parts that might be too narrow or too wide because of cardiospasm.
Another test used is a cine-esophagram. This test is a lot like the barium swallow. But instead of still pictures, the doctor takes a video of your esophagus with X-rays as you swallow. This gives a moving picture of your esophagus. It can show if the muscles in your esophagus are moving correctly. This is important for finding problems like aperistalsis that might be seen with cardiospasm.
All these tests, like high-resolution manometry, barium swallow, and cine-esophagram, help doctors get a good look at cardiospasm. They show whether it’s cardiospasm or something else. This is key for choosing the best treatment. And the right treatment means a patient can have a better life with cardiospasm.
Stem Cell Therapy for Cardiospasm
Stem cell therapy is showing promise for patients with cardiospasm. It aims to fix issues with the esophagus. This is done using the power of stem cells to grow new tissue.
Tests so far look good. Patients see a difference, feeling better and moving easier. This new way could change lives for those with cardiospasm.
But, more study is needed. We have to see if this treatment really works in the long run. Stem cell therapy might soon be a real choice for people needing to get their esophagus working right again.