Arthritis reactive, known as inflammatory joint disease, affects the joints and cartilage. It consists of diseases such as osteoarthritis and rheumatoid arthritis. They cause joint inflammation, possibly leading to pain, stiffness, and swelling.
When the immune system attacks the body by mistake, it causes autoimmune arthritis like rheumatoid arthritis. This leads to chronic inflammation and damages the joints. It’s important to manage arthritis symptoms to avoid flare-ups and find relief from joint pain.
Key Takeaways:
- Arthritis reactive is an autoimmune disease that affects joints and cartilage, causing joint inflammation and other symptoms.
- Osteoarthritis and rheumatoid arthritis are the most common types of arthritis.
- Proper diagnosis involves a combination of medical history, physical examination, and imaging tests.
- Treatment options include medication, physical therapy, and lifestyle changes.
- Stem cell therapy shows promise as a new approach to treating rheumatoid arthritis and improving patient outcomes.
Types of Arthritis and their Dangers
Arthritis comes in many types, each with unique symptoms and impacts. The most seen ones are osteoarthritis, rheumatoid arthritis, psoriatic arthritis, gout, and lupus arthritis.
Osteoarthritis shows as the wearing down of joint cartilage. This leads to pain, stiffness, and less movement. Rheumatoid arthritis, though, is an immune system problem. It attacks joints and causes swelling and damage.
People with psoriasis might also get psoriatic arthritis. It features red, scaly skin and joint issues. Gout happens when uric acid crystals build up in joints. This causes sharp pain, often in the big toe.
Lupus arthritis is linked to a disease that affects the whole body. It brings joint pain and swelling with it.
While arthritis won’t usually end your life, it can greatly harm your joints. The real risks are chronic pain and a lower quality of life. That’s why it’s crucial to treat and manage arthritis to avoid such issues.
Causes and Risk Factors of Arthritis
Arthritis is caused by many things, including genes, the environment, and the way we live. It’s important to know what causes and risks are tied to arthritis. This helps us deal with it and even stop it from happening.
Age
Getting older means you might get arthritis. Your joints wear out over time, making arthritis more likely to happen.
Injuries
Hurting your joints can lead to arthritis. If you’ve ever had a broken bone or tore a ligament, this could be why. It’s because these injuries can harm tissues around your joints, leading to more risk of arthritis.
Infections
Sometimes, arthritis is caused by infections. Illnesses like flu or sepsis can infect your joints. This can cause them to get swollen and damaged. It’s important to treat these infections early to avoid problems.
Obesity
Being overweight is another risk for arthritis. Extra weight strains your joints, especially the knees and hips. This can speed up how fast your joints wear out. Staying at a healthy weight can keep your joints working well.
Autoimmune Diseases
Illnesses where your immune system attacks your own body, like rheumatoid arthritis, can harm your joints. They cause swelling and damage in the joints.
Environmental Factors
Some things in the environment, like smoking or dirty air, can increase your chances of getting arthritis. These can cause swelling and joint damage over time.
| Causes of Arthritis | Risk Factors |
|---|---|
| Genetic predisposition | Age |
| Injuries | Joint injuries |
| Infections | Obesity |
| Autoimmune diseases | |
| Environmental factors |
By knowing and dealing with these causes and risks, we can better manage or prevent arthritis. This means making smart choices in how we live and getting the right medical help. Doing these things can help us avoid the worst impacts of arthritis on our lives.
Diagnosis of Arthritis
Diagnosing arthritis involves many steps, such as looking at your past health, checking your body, and running tests. This helps doctors see what kind of arthritis you have and how bad it is. They then decide on the best way to help you. Sometimes, they need to take a fluid sample from your joint to find out more.
Doctors start by asking you about your past health. They want to know if you’ve had any joint pain, stiffness, or swelling. They also ask about diseases in your family and any health risks you might have. This part is crucial for finding out what might be causing your symptoms.
After the talk, doctors will check your joints by moving them around and looking at them. They’re searching for signs like swelling or odd shapes. This exam helps them pick the most likely reasons for your joint problems.
Labs play a big part in diagnosing arthritis. They test for signs of swelling, autoimmune diseases, and other health issues linked to arthritis. Some tests they might order are full blood count, ESR, CRP, rheumatoid factor, and CCP antibodies.
Along with lab tests, pictures of your joints from X-rays, MRIs, or ultrasounds are also useful. These images show the inside of your joints, which can help spot damage or other problems. It gives doctors clear clues for a correct diagnosis.
Joint Fluid Aspiration
Sometimes, taking out some joint fluid for tests is necessary. This process is known as joint fluid aspiration. Doctors insert a needle into your joint to get a fluid sample. Then, this fluid is tested to look for infections, crystals, or more.
This test can tell a lot about what’s causing your arthritis, like an infection or a crystal buildup. Knowing the exact issue helps doctors plan the right treatment and confirm your diagnosis.
| Arthritis Diagnosis Methods | Benefits |
|---|---|
| Medical History | Provides insights into past symptoms, risk factors, and family history. |
| Physical Examination | Assesses joint function, identifies abnormalities, and determines the range of motion. |
| Laboratory Tests | Detects markers of inflammation, autoimmune diseases, and other underlying conditions. |
| Imaging Examinations | Visualizes joint structures, detects joint damage, and rules out other potential causes. |
| Joint Fluid Aspiration | Provides diagnostic insights into infection, crystal deposition, or autoimmune conditions. |
Blood Tests for Arthritis
Blood tests are key in checking and tracking arthritis. Doctors use them to look for signs of inflammation and autoimmunity. These tests give important information about a person’s health. This helps doctors pick the right treatment.
The rheumatoid factor test is often used for diagnosing rheumatoid arthritis. It looks for autoantibodies that attack the body, causing joint issues. A positive result can help confirm a diagnosis.
The antibodies to CCP test is also vital. It checks for antibodies linked to rheumatoid arthritis. It’s especially helpful if the rheumatoid factor test is negative.
The CRP test measures liver-produced substances during inflammation. High CRP levels mean there’s likely inflammation, common in arthritis.
The ESR test shows how fast red blood cells fall. High ESR levels suggest inflammation, common in arthritis too.
Doctors might also run other blood tests to get a full health picture. These can help find more inflammation or problems linked to arthritis.
For instance, the HLA-B27 test looks for a gene associated with some autoimmune diseases. It can help diagnose and treat conditions like ankylosing spondylitis.

Blood tests are critical for arthritis diagnosis and tracking. They reveal immune and inflammatory conditions. With these results, doctors can properly diagnose, treat, and manage arthritis.
Treatment of Arthritis
Treating arthritis depends on the kind and how bad it is, plus the patient’s health. Doctors usually suggest a mix of methods to handle symptoms and improve the patient’s life.
Medications
Medication is key in fighting arthritis pain and swelling. Doctors often prescribe NSAIDs to lower pain and inflammation. For some types of arthritis, like rheumatoid, special drugs called DMARDs can slow its progress.
Physical Therapy
Physical therapy helps by making joints move better, strengthening muscles, and boosting function. A therapist will create an exercise plan just for you. It might include exercises, strength building, and activities like swimming.
Auxiliary Devices
Devices like braces, splints, and orthotic shoe inserts can take pressure off sore joints. This makes moving easier and protects joints from more harm.
Weight Control
Keeping a healthy weight is vital if you have arthritis. Extra weight can hurt your joints more, causing more pain. By eating well and staying active, arthritis and your life can improve.
Surgical Treatment
Sometimes, surgery is needed to fix bad arthritis and help joints work better. If someone is really suffering, they might need a new knee or hip. But, surgery is only considered if nothing else works.
Lifestyle Modifications
Changing some habits can make a big difference in managing arthritis. Eating healthy and not smoking are important. Stress management and gentle exercises, like swimming or tai chi, also help.
Putting together these treatments, customized for each person, can make life much better for those with arthritis.
| Treatment Options | Description |
|---|---|
| Medications | Nonsteroidal anti-inflammatory drugs (NSAIDs) and disease-modifying antirheumatic drugs (DMARDs) are commonly used to reduce pain and inflammation. |
| Physical Therapy | Includes exercises to improve joint mobility, strengthen muscles, and increase overall function. |
| Auxiliary Devices | Braces, splints, canes, and orthotic shoe inserts provide support to reduce stress on affected joints. |
| Weight Control | Maintaining a healthy weight reduces stress on weight-bearing joints. |
| Surgical Treatment | Joint replacement surgeries such as knee replacement or hip replacement may be necessary for severe cases. |
| Lifestyle Modifications | Adopting a nutritious diet, quitting smoking, managing stress, and engaging in regular physical activity can help manage arthritis symptoms. |
Modern Treatment of Rheumatoid Arthritis with Stem Cells
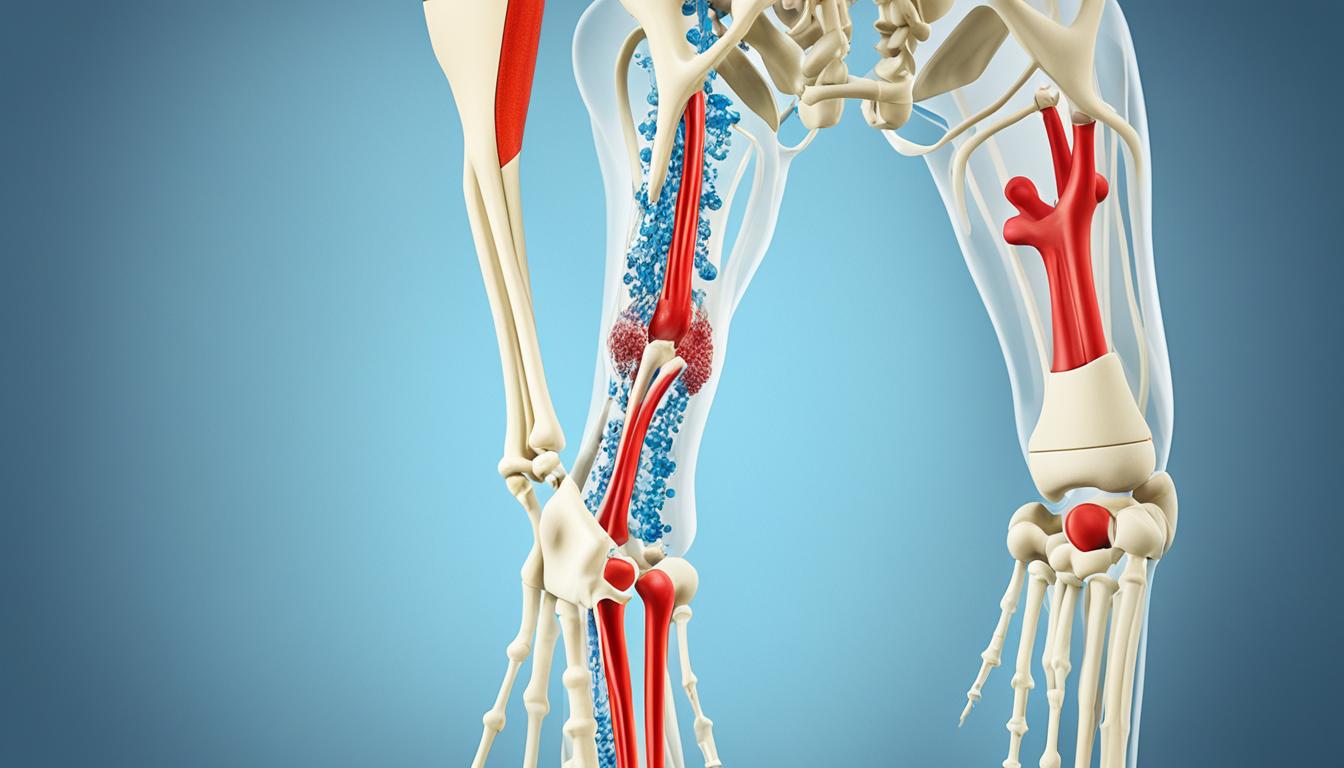
Recent research shows promise in using mesenchymal stem cells (MSCs) to treat rheumatoid arthritis. They have immunomodulatory traits and have been in both experimental studies and clinical applications. These cells can help regulate the immune system. They also aid in tissue repair by turning into healthy cells and stop inflammation. So, using MSCs could be a new and helpful way to treat rheumatoid arthritis and make the patients’ lives better.
Immunomodulation is key in stem cell therapy for this arthritis. MSCs can lower the immune system’s response, leading to less inflammation. They communicate through signals and by touching other cells. This includes immune cells such as T cells and B cells, changing their actions and reducing inflammation.
In studies, MSCs have shown the ability to lower harmful cytokines, like TNF-α and IFN-γ. They can also increase helpful cytokines, like IL-10 and TGF-β. These actions help bring back immune balance and limit the damage to joint tissues by rheumatoid arthritis.
Using stem cell therapy in real patients has also proven promising. In a small test, patients who got MSC injections saw their disease activity go down and their joint function improve. These results show MSCs might be a safe and really helpful treatment for rheumatoid arthritis.
MSCs for rheumatoid arthritis is a growing field. We still need more research to fully understand how it works and its long-term effects. Yet, MSCs’ power to adjust the immune response and their repair abilities offer a new hope for developing treatments for rheumatoid arthritis and similar conditions.
Future Directions in Stem Cell Therapy for Rheumatoid Arthritis
- Optimizing the delivery and dosage of MSCs
- Identifying biomarkers to predict treatment response
- Developing standardized protocols for MSC production and quality control
- Combining MSC therapy with other treatment modalities for enhanced efficacy
- Expanding clinical trials to assess long-term safety and effectiveness
Advancing in stem cell therapy is promising for people dealing with rheumatoid arthritis and even in the medical field. More research and innovation can greatly improve their lives.
Mechanism of MSCs in Suppressing the Immune System
Mesenchymal stem cells (MSCs) help suppress the immune system. They control various immune cells like T cells and B cells. Also, they affect NK cells, neutrophils, macrophages, and dendritic cells (DCs).
MSCs change T cells into regulatory T cells (Tregs). Tregs are important for immune balance and stopping autoimmune diseases. This helps lower inflammation.
MSCs also directly interact with B cells, NK cells, and others. This can calm down the immune system and lower inflammation.
MSCs slow down B cell growth and cut how much antibodies they make. They also decrease the power of NK cells, which helps avoid too much cell death.
MSCs stop neutrophils and macrophages from getting too active. These cells cause more damage during inflammation. So, MSCs help limit harm from inflammation.
Another way MSCs work is by affecting DCs. DCs start and control immune reactions. MSCs can slow down DCs, which helps control the immune system.
In short, MSCs are a promising treatment for auto and inflammatory diseases. They adjust immune cell activities and lower inflammation. This is key in the growing field of regenerative medicine.
Summary of MSCs’ Mechanisms in Suppressing the Immune System
| Immune Cell Population | Mechanism |
|---|---|
| T cells | Differentiation into regulatory T cells |
| B cells | Inhibition of proliferation and antibody production |
| NK cells | Suppression of cytotoxic activity |
| Neutrophils | Inhibition of activation |
| Macrophages | Inhibition of activation |
| DCs | Inhibition of maturation and activation |
MSCs play a big role in changing the immune system. They could be key in treating issues like inflammation and autoimmune diseases.
Conclusion
Stem cell therapy, with a focus on mesenchymal stem cells (MSCs), shows a lot of promise in treating autoimmune diseases like rheumatoid arthritis. MSCs work by balancing the immune system and helping with tissue repair. This is different from the usual medicines we use.
We are excited about MSCs and how they can help with arthritis and other autoimmune illnesses. But we still need more studies and trials to be sure they are safe and work well. Learning more about MSCs will show us how they can really help in rheumatology.
Stem cell therapy might change the game in rheumatology, bringing better results for patients. It could offer new hope to those with autoimmune diseases. The new methods with MSCs show great promise for handling these tough health problems.
Regenerative medicine, like stem cell therapy, gives us hope for treating autoimmune diseases better. With more research, we’re getting closer to a day when stem cell therapy could really help people with arthritis and similar conditions. The work being done is moving us towards that hopeful future.