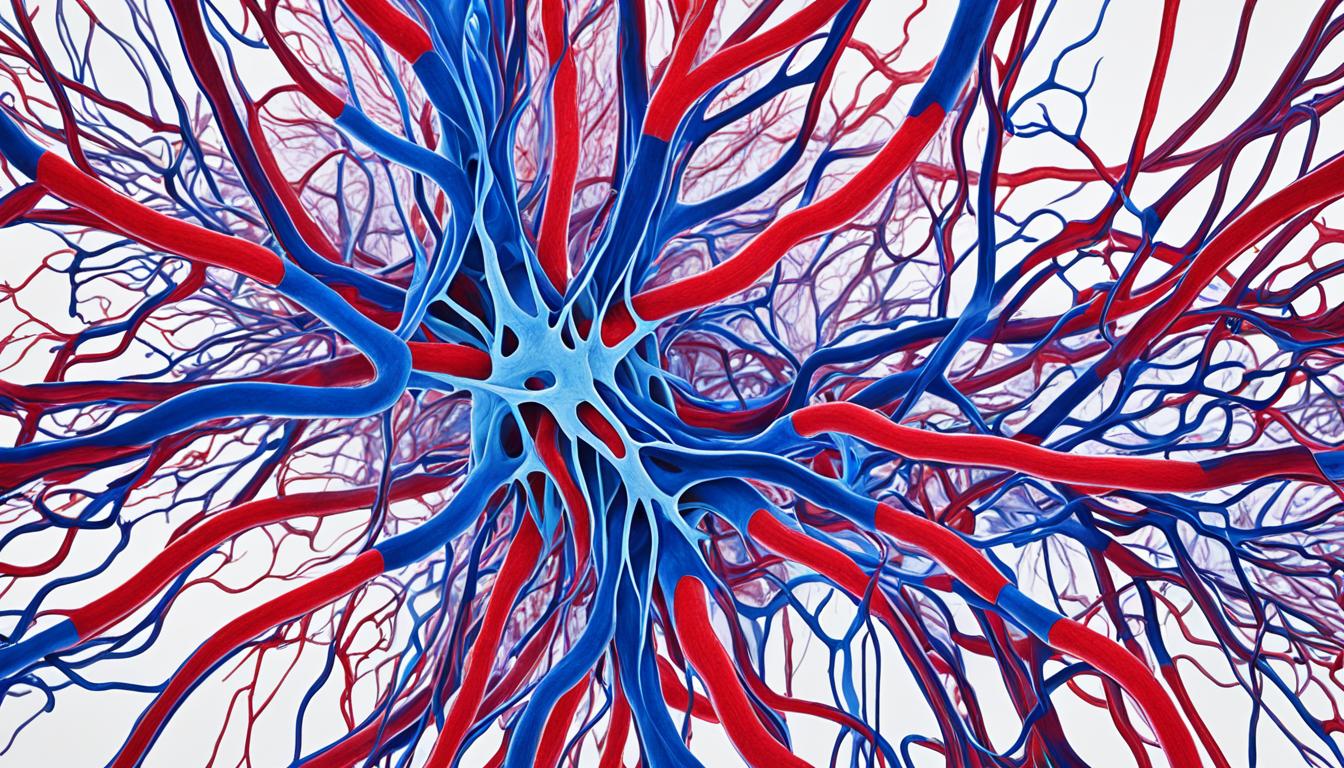
Arteriovenous malformations (AVMs) affect blood vessels, especially in the brain. They are like tangled webs of blood vessels. This disrupts how blood and oxygen travel to tissues. Some AVMs never cause problems, but others can harm tissues, cut off oxygen, or burst.
The size and location of AVMs affect their impact. They might cause seizures, headaches, and weak muscles. For some, thinking and understanding become harder. If AVMs get bigger, they can press on parts of the brain or spine. Knowing about AVM symptoms and care helps treat those affected.
Key Takeaways:
- Arteriovenous malformations (AVMs) are blood vessel problems that affect blood and oxygen flow.
- They can damage tissues, cause oxygen loss, and might lead to a burst blood vessel.
- AVMs bring a range of problems, from seizures and headaches to muscle weakness and trouble thinking.
- Doctors can find AVMs with scans. Treatment choices depend on the AVM type, where it is, and the symptoms.
- Stem cell therapy is in the early stages of testing for AVMs.
Keeping up with AVM understanding and treatment progress is vital for both doctors and patients. We’ll explore more on AVMs, covering symptoms, risks, how they’re found, treated – including potential new therapies.
What are Arteriovenous Malformations?
Arteriovenous malformations (AVMs) are tangled blood vessels that mix up the blood flow. They’re most often found in the brain and spinal cord. These abnormal mix-ups can lead to serious issues.
AVMs are missing a key part, capillaries. Capillaries usually help blood get oxygen before it reaches other tissues. Without them, blood goes straight from arteries to veins. This misses out on the important step of oxygenating the blood. The lack of oxygen can harm tissues, kill nerve cells, and damage other cells.
Some AVMs stay small and don’t cause symptoms. But, as they get bigger, problems can arise. The size and location of the AVM can affect how serious the situation is.
When an AVM is in the brain or spinal cord, it’s especially risky. These areas are vital for our health. Getting a diagnosis quickly and choosing the right treatment is very important. It helps prevent serious issues caused by AVMs.
Symptoms of Arteriovenous Malformations
Arteriovenous malformations (AVMs) bring various symptoms of different intensity and types. These may include:
- Seizures: AVMs can cause sudden and uncontrolled movements.
- Headache: Frequent and severe headaches are common.
- Pain: Pain might be felt in the head or specific body part.
- Visual problems: Issues like blurred or double vision can happen.
- Muscle weakness: Weakness or paralysis in muscles may occur.
- Speech problems: Speech may become slurred or hard to understand.
- Movement difficulties: Coordination and balance problems are possible.
- Abnormal sensations: People might feel numbness or tingling in their body.
- Cognitive difficulties: Memory issues, trouble focusing, or thinking problems are signs.
- Dizziness: Dizziness or feeling like the room is spinning can happen.
- Loss of consciousness: Some might faint or lose consciousness.
- Developmental differences: In kids, AVMs might slow development.
The signs rely on where the AVM is in the brain or spine. Remember, head pain’s location doesn’t always show the AVM’s exact spot. Symptoms can start at any age but are more usual in people over 20. Pregnancy might make symptoms worse. This is because changes in blood flow and pressure affect the AVM more.
Knowing these symptoms helps for early diagnosis and the right medical care. This lessens the risks linked with AVMs.
Risk of Hemorrhage in Arteriovenous Malformations
Arteriovenous malformations (AVMs) can cause dangerous bleeding. Smaller AVMs are more likely to bleed. If an AVM has bled before, it’s likely to bleed again within a year. AVMs that block blood from draining, like by narrowing or clogging veins, are at higher risk of severe bleeding.
AVMs deep inside the body can cause more damage than those closer to the surface. Pregnancy can increase the risk of bleeding. This is because blood pressure and volume change during pregnancy.
A severe type of AVM is called the vein of Galen malformation. It shows up in newborns and infants. Catching it early is crucial to prevent severe bleeding and its effects.
Factors Contributing to Hemorrhage Risk in AVMs
Many things can affect how likely an AVM is to bleed:
- The AVM’s size
- If it has bled before
- Its location and how deep it is
- If it blocks blood from draining
- If you’re pregnant
- The presence of a vein of Galen malformation
| Type of AVM | Hemorrhage Risk |
|---|---|
| Small AVMs | Higher risk of bleeding |
| Previously hemorrhaged AVMs | Increased likelihood of recurrent bleeding |
| Deeply located AVMs | More severe damage potential |
| AVMs impairing drainage | Heightened risk of serious hemorrhage |
| Pregnancy | Elevated risk due to blood pressure and volume changes |
How Arteriovenous Malformations Damage the Brain and Spinal Cord
Arteriovenous malformations (AVMs) can harm the brain and spinal cord badly. They affect the way blood flows, causing damage and complications.
AVMs decrease the oxygen reaching the tissues. Normal vessels use capillaries to distribute oxygen. However, AVMs connect arteries and veins directly, causing oxygen and nutrients to be distributed poorly. Tissues can lack oxygen, leading to their decay or death.
AVMs are also linked to bleeding in the tissues. The fast blood flow damages vessel walls, leading them to break. This breaks can cause bleeding and harm the tissues around them.
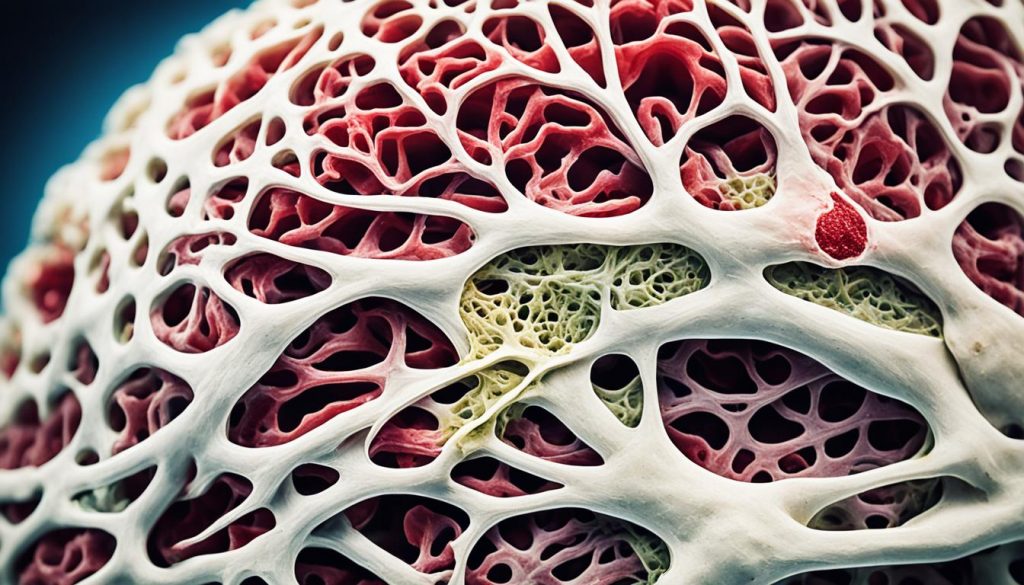
In addition, big AVMs might press on brain parts. This pressure can deform or move these parts, causing issues like hydrocephalus. It also puts pressure on key parts of the brain and spinal cord.
These impacts on the brain and spine can be severe. It is important to diagnose AVMs early and treat them promptly. This helps to avoid serious damage and life-threatening problems.
Effects of Arteriovenous Malformations on the Brain and Spinal Cord
| Effect | Description |
|---|---|
| Tissue Damage | AVMs disrupt oxygen and nutrient delivery to the tissues, causing them to become oxygen-depleted and deteriorate or die. |
| Bleeding | The rapid blood flow and weakened vessel walls of AVMs can lead to ruptures and bleeding into the surrounding tissues. |
| Compression of Brain Structures | Large AVMs can compress or displace brain structures, potentially leading to complications like hydrocephalus and increased pressure on neurological tissues. |
Arteriovenous Malformations vs. Other Vascular Lesions
Arteriovenous malformations (AVMs) are not the same as aneurysms, hemangiomas, or fistulas. Knowing these differences helps doctors make the right choice for treatment.
1. Aneurysms
Aneurysms are weak spots in arteries’ walls. They’re different from AVMs because they’re bulges in the blood vessels that can burst and cause a serious problem.
2. Hemangiomas
Unlike AVMs that can be in the brain, hemangiomas are on the skin’s surface. Usually, they don’t need treatment as they’re not harmful.
3. Cavernous Malformations
Cavernous malformations are in the brain or spine. They are clusters of blood vessels not fast-flowing like AVMs, often not causing big issues.
4. Fistulas
Fistulas are abnormal blood vessel connections. They might be from head injuries or infections and are found in the brain’s coverings or the spine. AVMs usually appear inside the brain tissue.
It’s key to spot AVMs apart from other vascular problems for the right treatment. Each type has its own traits and needs special care.
| Condition | Description |
|---|---|
| Aneurysms | Weakened areas in artery walls; risk of rupture and bleeding |
| Hemangiomas | Benign vascular malformations on the skin; do not require treatment |
| Cavernous Malformations | Slow-flow vascular lesions; enlarged blood vessels |
| Fistulas | Abnormal connections between blood vessels; associated with head trauma or infections |
Diagnosis and Treatment of Arteriovenous Malformations
Doctors find arteriovenous malformations (AVMs) by using special tests. They look for these when someone has certain symptoms. Imaging tests help by showing the abnormal blood vessels. They also show where the AVM is and how big it is.
- Magnetic Resonance Imaging (MRI) looks at the brain closely with a magnetic field and radio waves.
- Computed Tomography (CT) Scan combines several X-rays to see inside the body in 3D.
- Cerebral Angiography uses a dye to look at the brain’s blood vessels in detail.
After finding an AVM, doctors create a plan just for that person. The best treatment depends on where the AVM is, its size, and the symptoms the person has. Also, the patient’s health is taken into consideration. The main ways to treat AVMs are:
- Surgery: Surgeons can remove the AVM. They cut off the extra blood vessels to help blood flow go back to normal. This is a common choice for smaller AVMs that are easy to reach.
- Radiation Therapy: High-energy rays can be aimed at the AVM to make it smaller or get rid of it. Doctors use this for AVMs that are deep or hard to operate on, or if surgery is too risky.
- Embolization: Doctors can use a thin tube called a catheter to put special things into the blood vessels that feed the AVM. This stops or lessens the blood flow. It’s usually done before surgery or radiation to help these treatments work better.
New treatments for AVMs are also being looked into. One exciting option is stem cell therapy. This could help repair the area by growing into different types of cells.
Knowing all your AVM treatment choices is very important. Patients should talk a lot with their doctors. Ask questions and understand the good and bad of each treatment. Choosing wisely about one’s health care can really help with AVMs.
| Treatment Option | Description |
|---|---|
| Surgery | Removal of the AVM through a surgical procedure. |
| Radiation Therapy | High-energy beams are used to destroy or shrink the AVM. |
| Embolization | Special materials are used to block or reduce blood flow to the AVM. |
Genetic Factors and Risk of Arteriovenous Malformations
Arteriovenous malformations (AVMs) are complex and rare. They can be influenced by our genes. Different genes that involve inflammation, matrix metalloproteinases, and cytokines can increase the risk of AVMs and their problems.
Changes in genes linked to inflammation can lead to AVMs. Our body’s response to inflammation helps these malformations grow. Thus, genes that handle inflammation can affect our AVM risk.
Matrix metalloproteinases (MMPs) help change blood vessels’ structure. If genetic changes affect MMPs, the risk of AVMs rises. Problems with these enzymes can cause blood vessels to form abnormally and AVMs to develop.
Cytokines control how cells work, including inflammation and blood vessel growth. Genetic changes that impact cytokines can raise the chances of getting AVMs. When cytokines work incorrectly, it can mess up how blood vessels develop, leading to AVMs.
Finding out the genetic links with AVMs is vital for better diagnoses and treatments. Knowing the specific genes and variants tied to AVMs helps with risk assessment and finding them early. This can lead to treatment plans tailored to the individual.
Risk Factors Associated with Genetic Variations
| Genetic Factors | Risk for AVMs |
|---|---|
| Inflammation-related gene variations | Increased risk |
| Matrix metalloproteinase gene variations | Increased risk |
| Cytokine-related gene variations | Increased risk |
Future Research and Implications
Research is focused on understanding AVMs better and finding new treatments. Scientists and doctors are working hard to help those with this condition.
Stem cell therapy shows a lot of promise. It aims to use stem cells to repair tissues and build new, healthy blood vessels. This could be a key part of treating AVMs in the future.
Genetic studies are also a big part of the research. They look for links between specific genes and AVMs. This could help predict how the disease might develop in a person. It may also lead to treatments more suited to each patient’s needs.
Another focus is on finding treatments that target the causes of AVMs. The goal is to use what we know about the disease to stop it from getting worse. Researchers are looking at specific ways to treat or even reverse AVMs. This could change how this condition is managed in the future and make patient outcomes better.
Implications of Future Research
Research in AVMs could greatly change how we diagnose and treat them. Progress in stem cell therapy and genetic studies may lead to treatments that are more effective and fit each patient better. This would mean a big improvement in the lives of those with AVMs.
Developing treatments that target the root causes of AVMs could also make treatments safer and more effective. By tackling the main issues behind AVM development, these methods might offer better options than what’s available now.
| Research Focus | Impact |
|---|---|
| Stem Cell Therapy | Potential regenerative treatment option |
| Genetic Studies | Improved risk prediction and personalized interventions |
| Targeted Treatments | Potential prevention and reversal of AVMs |
It’s key to remember that this research is still ongoing. We need more studies to make sure these new treatments are both safe and effective. But, these efforts give us hope for managing AVMs better in the future. They take us closer to truly understanding and treating this disease.
Conclusion
Arteriovenous malformations (AVMs) are complex vascular abnormalities. They pose serious risks by causing abnormal tangles of blood vessels. These tangles can disrupt artery-vein connections, leading to critical health threats. For patients and healthcare providers, knowing about AVMs’ symptoms, causes, diagnosis, and treatments is key.
Tackling AVMs is challenging but there are effective treatment options. These include surgeries, radiation therapy, and embolization. Such methods help in managing AVMs and decreasing complications. Luckily, research and advancements offer promise for better treatments in the future.
One promising area is stem cell therapy, which holds potential in AVM treatment. It aims to repair damaged tissues and improve AVM management. Moreover, genetic studies are revealing critical genes and mutations linked to AVMs. This knowledge enhances risk assessment and tailors treatments for each patient.
Advances in stem cell therapy and genetic research are key to enhancing AVM care. Collaboration among healthcare providers, researchers, and patients is vital. Together, they can push for improved diagnostics, personalized treatments, and a deeper grasp of AVM complexities. This unified effort is crucial for better outcomes in AVM cases.