Angiofollicular lymph node hyperplasia, also known as Castleman disease, is rare. It affects different parts of the body by enlarging lymph nodes. The condition has two types: unicentric and multicentric.
Unicentric Castleman disease shows up in the chest area as a single mass. It’s often found by chance during check-ups. In contrast, the multicentric type links with HIV and causes more severe issues like fever, night sweats, and weight loss.
The real cause behind Castleman disease is still a mystery. Experts think it’s tied to long-term mild inflammation. Doctors usually confirm it by checking an enlarged lymph node with a biopsy. Common treatments are surgery, chemo, and medications like prednisolone. For harder-to-treat cases, stem cell therapy might be a choice.
Key Takeaways:
- Angiofollicular lymph node hyperplasia, or Castleman disease, is a rare lymph condition marked by big lymph nodes.
- There are two types of Castleman disease: unicentric and multicentric. Unicentric type comes as a single mass, and the multicentric type shows up with serious symptoms and HIV.
- The cause of Castleman disease is not fully understood but may involve long-term mild inflammation.
- Doctors diagnose it by checking lymph nodes. Treatments range from surgery to stem cell therapy.
- If standard treatments don’t work, some patients might consider stem cell therapy.
What is Angiofollicular Lymph Node Hyperplasia?
Angiofollicular lymph node hyperplasia, also called Castleman disease, is a rare issue. It leads to the abnormal growth of lymph nodes. They grow larger than usual. Most often, they form a single mass in the chest area.
This disease is marked by increased blood supply to these large nodes. There are two types: one affects just one lymph node (unicentric), and the other affects several (multicentric).
The exact reason for Castleman disease is not clear. But, it’s linked to ongoing swelling. Symptoms depend on the type. Unicentric Castleman often has no symptoms and is found by chance. Multicentric can bring fever, night sweats, and tiredness.
To diagnose Castleman disease, doctors use a biopsy. This involves taking out a piece of the affected node for testing. Various scans help to see the nodes better.
For treatment, options like surgery, chemo, or medicines are available. Some newer treatments that target specific parts of the immune system show promise. In hard cases, stem cell therapy might be suggested. This happens after a strong round of chemo, using the patient’s own cells.
It’s crucial to keep an eye on the disease over time. This can ensure the best outcome. Understanding Castleman disease is key. It helps doctors offer the right care to those who have it.
| Key Points |
|---|
| Angiofollicular lymph node hyperplasia, or Castleman disease, is a rare lymph issue. |
| The disease can occur in various places in the body. The chest is most common. |
| It comes in two types: unicentric, affecting one node, and multicentric, more than one. |
| The exact cause is not fully known but it seems to be linked to ongoing swelling. |
| Diagnosis is done by testing tissue from a node, taken through a biopsy. |
| Treatments include surgery, chemo, certain medicines, and new therapies focused on the immune system, and if needed, stem cell therapy. |
| Outlook differs based on the type of disease and other factors for each patient. |
Symptoms of Angiofollicular Lymph Node Hyperplasia
The symptoms of angiofollicular lymph node hyperplasia change based on the disease type. Castleman disease has different subtypes, each with its own symptoms.
Symptoms of Unicentric Castleman Disease:
People with the unicentric subtype often have no symptoms. Their disease is found by chance during check-ups. But, if an enlarged lymph node doesn’t hurt, that might be a sign. This is called painless lymphadenopathy.
Symptoms of Multicentric Castleman Disease:
The multicentric type shows more wide-ranging symptoms. This can include:
- Fever: Patients may experience persistent or recurrent fevers.
- Night sweats: Excessive sweating during the night, which can lead to discomfort and disrupted sleep.
- Fatigue: Patients may feel excessively tired and lack energy.
- Weight loss: Unexplained weight loss can occur, even without changes in diet or physical activity.
Also, it can lead to enlarged lymph nodes all over the body. There might be a swelling of the liver and spleen, along with retaining fluids. Blood issues, like anemia, are common too, in this type of Castleman disease. They often have higher levels of inflammation markers and certain blood proteins, along with low albumin.
| Symptom | Unicentric Castleman Disease | Multicentric Castleman Disease |
|---|---|---|
| Asymptomatic | ✓ | – |
| Painless lymphadenopathy | ✓ | – |
| Fever | – | ✓ |
| Night sweats | – | ✓ |
| Fatigue | – | ✓ |
| Weight loss | – | ✓ |
| Generalized lymphadenopathy | – | ✓ |
| Hepatosplenomegaly | – | ✓ |
| Fluid retention | – | ✓ |
Causes of Angiofollicular Lymph Node Hyperplasia
Angiofollicular lymph node hyperplasia, known as Castleman disease, has a mysterious cause. It’s linked to ongoing low-grade inflammation. This disease has two forms: unicentric and multicentric.
The unicentric type often shows no symptoms and is accidentally found. In contrast, the multicentric form connects to HIV. Studies show that HIV patients with multicentric Castleman disease also carry the human herpesvirus 8 (HHV-8).
For those with multicentric Castleman disease, other contributing factors include POEMS syndrome, osteosclerotic myeloma, Kaposi sarcoma, AIDS, amyloidosis, and chordoid meningioma.
These causes play a big role in the growth of angiofollicular lymph node hyperplasia. But, we still need more research to truly grasp why this rare disease occurs.
Diagnosis of Angiofollicular Lymph Node Hyperplasia
Diagnosis of angiofollicular lymph node hyperplasia, or Castleman disease, uses various methods. The key way to diagnose it is by removing a lymph node and examining it. If this is not possible, doctors might use a small needle to take a sample for testing.
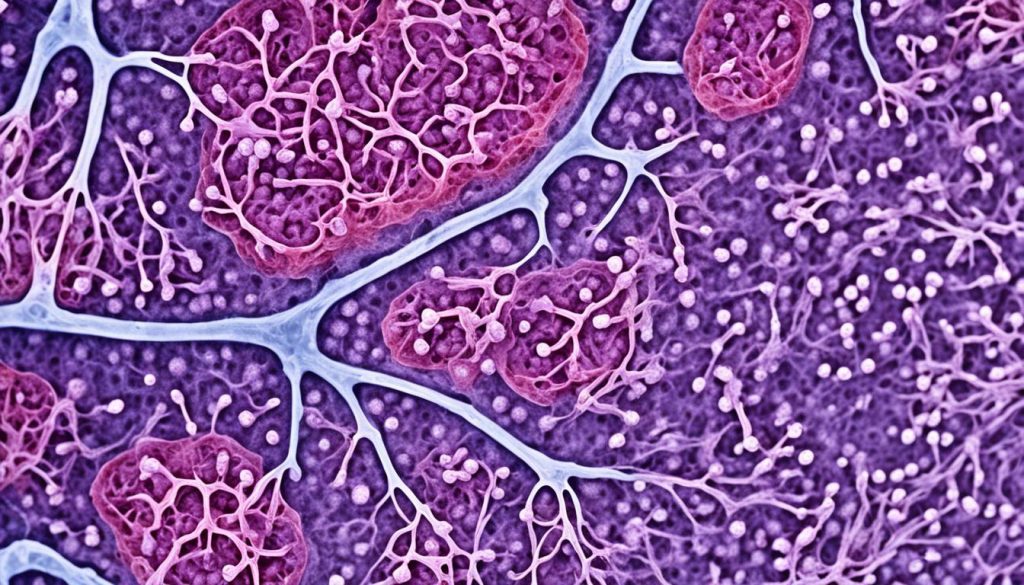
Doctors look at the lymph node under a microscope in a process called histopathological analysis. This helps them see the specific features of the disease and identify its type, like the subtype.
Angiofollicular lymph node hyperplasia may have different subtypes. These include:
- Hyaline vascular subtype: Shows more hyalinized blood vessels in and around follicles.
- Plasma cell subtype: Has crowded follicles in a lymph node region, often found in the multicentric subtype.
- HHV-8-associated subtype: Connected to a virus called human herpesvirus 8 (HHV-8).
- Multicentric Castleman disease not otherwise specified: A subtype with less clear characteristics.
Imaging tests like ultrasound, CT scans, MRI, and PET scans are also used. These tests help to see the lymph nodes better. They can show which lymph nodes are larger, helping with the diagnosis.
By using information from various tests, doctors are able to diagnose this disease. They can then decide on the best treatment for the patient.
Treatment of Angiofollicular Lymph Node Hyperplasia
The way we treat angiofollicular lymph node hyperplasia, or Castleman disease, varies. It depends on the type and how bad the disease is. Treatments include:
- Surgery: Surgery is the top option for unicentric Castleman disease. It involves cutting out the swollen lymph node. This can cure the disease in a lot of cases.
- Chemotherapy: For multicentric Castleman disease, chemotherapy is often needed. This type affects many lymph nodes. Chemotherapy can help stop the cells from growing wrong and lessen symptoms.
- Prednisolone: Prednisolone is a type of medicine that fights inflammation. It is used for Castleman disease because it helps calm down the immune system. This makes symptoms better.
- Antiviral strategies: If Castleman disease is linked to HHV-8, special antiviral treatments can be used. These aim to beat the virus and control the disease better.
- Monoclonal antibody therapies: Doctors can also use specific antibodies for this disease. They may target CD20 or IL-6. This is when other treatments don’t work well.
When the first-line treatments don’t work, some patients might need a different approach. This includes using their own stem cells to help fix their immune system. The process starts by collecting these cells from the blood. Then, after intense chemo, the cells are put back. This method has helped some with more severe forms of the disease.
The outlook for Castleman disease depends on how severe it is. Unicentric Castleman disease often gets better, especially with surgery. Still, dealing with the multi-lymph node form can be tougher. It may need more treatments mixed up together.
Stem Cell Therapy for Angiofollicular Lymph Node Hyperplasia
For people with multicentric Castleman disease and POEMS syndrome, some standard treatments might not work. So, doctors may suggest stem cell therapy. This approach involves using the patient’s own stem cells.
The stem cells are taken from the person’s blood. Then, after intense chemotherapy, they are put back into the body. The main aim is to help the immune system work better by using the power of stem cells.
Research shows good results for stem cell transplants in these diseases. They can help people go into long-term remission. This makes their health outlook and quality of life better.
Using stem cell therapy for angiofollicular lymph node hyperplasia shows the big promise of regenerative medicine. There’s excitement that new stem cell tech will bring even better ways to treat rare diseases in the future.
Epidemiology of Angiofollicular Lymph Node Hyperplasia
Overview
Castleman disease, or angiofollicular lymph node hyperplasia, is rare, affecting about 20 people in every million yearly. It’s seen more in adults but can occur in all ages. This disease has two forms. One impacts a single lymph node, and the other affects many. Not much is known about how common it is.
Incidence and Demographics
People usually get diagnosed with the single-node type, called unicentric, in their 30s or 40s. It’s a bit more common in females. With a mass in the chest, it often shows no symptoms. The multiple-node type, multicentric, appears later in life, mainly in the 50s or 60s. It’s found more in males and comes with other health problems. In some cases, it’s linked to HIV.
Prevalence and Geographic Distribution
Because it’s so rare, we don’t know how many people have angiofollicular lymph node hyperplasia. It’s thought to be found worldwide, affecting people of all races. Yet, more study is needed on where it’s most common and how many it affects.
Epidemiological Data
| Characteristic | Unicentric Castleman Disease | Multicentric Castleman Disease |
|---|---|---|
| Incidence | Estimated at 20 cases per million people per year | Unknown |
| Median Age at Diagnosis | 3rd and 4th decades | 5th and 6th decades |
| Gender Predominance | Slight female predominance | Slight male predominance |
Histological Types of Angiofollicular Lymph Node Hyperplasia
Castleman disease has distinct histological types. It’s important to know these for the right diagnosis and treatment. The most common type is hyaline vascular, found in 90% of unicentric cases[^1^]. It shows more tiny, glass-like blood vessels in and around lymph nodes. There’s also a special pattern of lymphocytes around the germs in these nodes[^2^].
Another type is the plasma cell variant, often seen in multicentric cases[^3^]. This variant has enlarged lymph nodes with clear channels. It has a lot of plasma cells in the middle and around them[^4^].
We also have other types, like HHV-8-linked and unspecified multicentric Castleman disease[^5^]. They all have their own unique characteristics. These help doctors understand the disease better.
Histological Types of Angiofollicular Lymph Node Hyperplasia
| Histological Type | Key Features |
|---|---|
| Hyaline vascular variant |
|
| Plasma cell variant |
|
| HHV-8-associated Castleman disease | Presence of HHV-8 in affected lymph nodes |
| Multicentric Castleman disease not otherwise specified | Additional features distinct from other histological types |
Finding the right histological type is key. It determines the best treatment and helps predict what the disease might do. Looking at the tissues closely under a microscope is critical for diagnosing Castleman disease. This process reveals a lot about what’s happening in the body.
Imaging of Angiofollicular Lymph Node Hyperplasia
Imaging methods are key to spotting big lymph nodes in angiofollicular lymph node hyperplasia cases. We use several ways to see this, like ultrasound, CT scans, MRIs, and PET scans. Each method gives us helpful info about where these nodes are, their size, and what they look like. This helps doctors diagnose and plan treatment accurately.
CT and MRI scans tell us a lot about these swollen lymph nodes. CT scans show details like shape and density. MRIs show more about the soft tissues and can spot if anything around these nodes has changed. They can even see if parts next to these nodes are inflamed or have grown extra bone.
PET scans, especially when done with FDG, offer unique benefits. They can tell if the disease is in one area or many. Plus, they measure how active these lymph nodes are. This helps see if the treatment is working and guides doctors on what to do next.
| Imaging Modality | Advantages | Limitations |
|---|---|---|
| Ultrasound | Safe, non-invasive, real-time imaging, low cost | Operator-dependent, limited ability to evaluate deep-seated lymph nodes |
| CT | High-resolution imaging, superior morphological detail | Ionizing radiation, contrast agent use |
| MRI | Superior soft tissue contrast, multiplanar imaging | Longer scan times, contraindicated in certain patients |
| PET | Metabolic information, whole-body imaging | Expensive, limited spatial resolution, requires radioactive tracer |
Prognosis of Angiofollicular Lymph Node Hyperplasia
The outlook for unicentric Castleman disease is usually good. Surgery can cure it in most situations. Still, people should watch for the disease coming back or getting worse over time.
The forecast for multicentric Castleman disease is not as promising. It’s harder to treat and may need more than surgery. This could include chemo, prednisolone, and, in some cases, stem cell therapy. How well someone responds to treatment depends on the kind and how severe their disease is, and their own health. Close medical care and watching the disease are key to leading a good life.
Prognosis Comparison:
| Prognosis Factors | Unicentric Castleman Disease | Multicentric Castleman Disease |
|---|---|---|
| Treatment | Surgical excision | Combination of surgery, chemotherapy, and prednisolone |
| Remission | Curative in most cases | Might require stem cell therapy if standard treatments fail |
| Prognosis | Generally good | Relatively poorer |
| Long-term Monitoring | Recommended to monitor for recurrence or progression | Close medical management is important for optimizing prognosis |
Looking at the table, it’s clear that unicentric Castleman disease has a better outlook than the multicentric type. For unicentric cases, surgery is often enough. Multicentric Castleman disease, on the other hand, needs different treatments and more careful medical attention. Sometimes, people may need stem cell therapy if the regular treatments don’t work. For both types, keeping a close eye on the disease is vital. It helps to make sure patients have the best possible chances of living well.
Conclusion
Castleman disease is a rare condition that can cause lymph nodes to grow abnormally. There are two main types: unicentric and multicentric. The unicentric type may not show any symptoms, but the multicentric type usually has symptoms that affect the whole body.
To diagnose it, doctors typically do an excisional biopsy of a swollen lymph node. Treatments can include surgery, chemotherapy, and medications like prednisolone. If these don’t work, they might suggest stem cell therapy.
If someone has the unicentric type, they often do well after treatment. But, they should check in with their doctors regularly. For those with the multicentric type, the outlook is not as good. They need careful monitoring and follow-ups to manage the disease and live well.

