Achalasia is a rare condition that affects how the esophagus works. It stops the muscles in the esophagus from relaxing properly after swallowing. This makes it hard for food to move from the esophagus to the stomach. People with achalasia might find it hard to swallow, spit up food, lose weight, and feel chest pain sometimes.
We are not sure what causes achalasia, but it could be linked to a viral infection in people with a certain genetic makeup. Doctors use several tests to diagnose it, including a barium swallow and an esophageal manometry.
There are different ways to manage achalasia, from changing your lifestyle to using medicine or undergoing surgery. Newer treatments like injecting botulinum toxin or using stem cell therapy are also being explored. But more studies are needed to know if these are safe and really work.
It’s important to understand achalasia’s signs, why it happens, how it’s diagnosed, and the ways it can be treated. With ongoing research and the development of better treatments, we can offer more hope to those dealing with achalasia.
Key Takeaways:
- Achalasia is a rare esophageal motility disorder characterized by the obstruction of food passage from the esophagus to the stomach.
- Symptoms of achalasia include difficulty swallowing, regurgitation, weight loss, and occasional chest pain.
- The exact cause of achalasia is unknown, but it is believed to be triggered by an environmental factor, possibly a viral infection.
- Diagnosis involves a combination of clinical evaluation, a barium swallow test, and esophageal manometry.
- Treatment options include lifestyle modifications, medications, endoscopic therapies, surgical interventions, and the potential use of stem cell therapy.
Achalasia Epidemiology and Demographics
Achalasia is a rare problem that affects the way the tube from your throat to your stomach works. It can be seen all over the world. Learning about how common it is and who it affects helps doctors and researchers understand it better.
Prevalence
It’s hard to put a number on how many people have achalasia. But, it’s guessed that about 1 in every 100,000 people might experience it. This shows that achalasia isn’t very widespread.
Age of Onset
Achalasia might show up at any age. But, it’s usually found in people between 25 and 60. This is the time when most cases are first noticed.
Gender Distribution
Both men and women are affected by achalasia at similar rates. The disease doesn’t seem to target one gender more than the other.
Demographic Distribution
This condition can pop up in anyone, regardless of geography or ethnicity. It’s rather uncommon, making up just a tiny fraction of esophageal issues.
Summary
Achalasia is a rare but global issue in the world of digestive health. It’s roughly found in 1 out of 100,000 people and often appears between ages 25 and 60. It doesn’t pick sides between men and women, nor does it favor any particular area or ethnic group. Knowing these details is crucial for healthcare workers to help those dealing with achalasia properly.
| Key Points |
|---|
| Achalasia is estimated to affect approximately 1 in 100,000 individuals. |
| The condition is most commonly diagnosed between the ages of 25 and 60. |
| Achalasia affects both males and females equally. |
| Achalasia is a relatively rare condition, accounting for less than 1% of all esophageal disorders. |
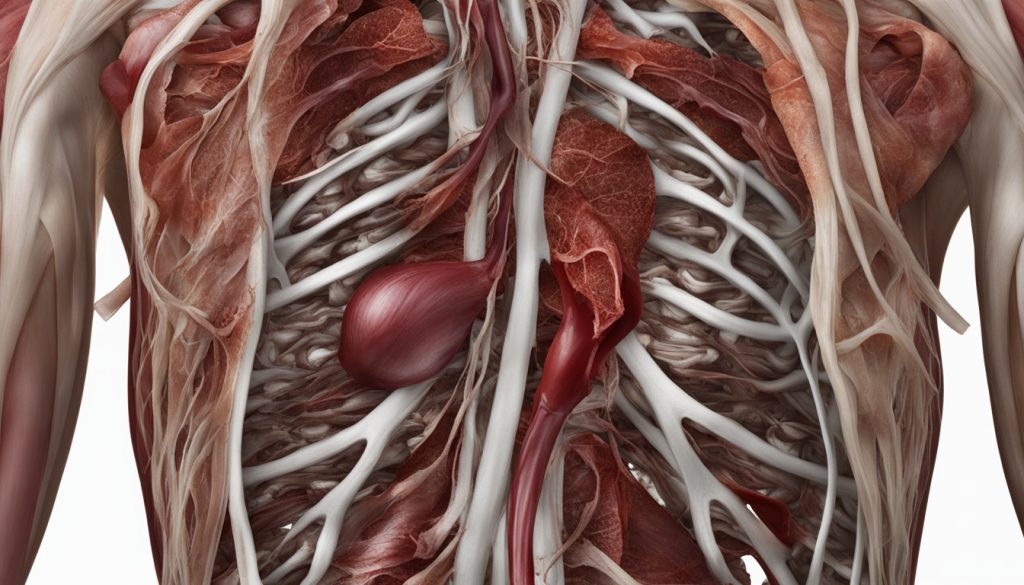
Achalasia Pathophysiology
The pathophysiology of achalasia is complex. It involves a specific loss of function in the lower esophageal sphincter. This makes it hard for food to move from the esophagus to the stomach. The exact cause of this is not clear. It’s thought to be due to something in the environment that affects people with a certain genetic makeup. This something might be a viral infection. This mix leads to damage in the esophagus, causing the typical achalasia signs.
Researchers are still figuring out what causes achalasia. But, they know that a problem with the lower esophageal sphincter is a big part. This issue makes it difficult for food to pass through the esophagus.
Achalasia Clinical Presentation and Diagnosis
Achalasia shows itself in various ways, most evident in trouble swallowing and digesting food. Mainly, people find it hard to swallow solid food and liquids, which is called dysphagia>. Over time, this can get worse, leading to weight drop.
People with achalasia might also throw up food that’s not digested. This happens because the muscle at the end of the esophagus doesn’t relax fully, blocking food from going down. Sometimes, there’s chest pain too, but it’s not as common as other symptoms.
Diagnosing it involves both evaluations by a doctor and special tests. A key test is the barium swallow test. Here, a person drinks a barium solution, then X-rays show how the esophagus works. If a person has achalasia, the X-rays might show a wider esophagus and a narrow, “bird beak” end.
Another critical test is esophageal manometry. It checks how the esophagus squeezes food down. A small tube goes through the nose to the esophagus for this test. It helps to rule out other esophagus problems and spot achalasia’s unique signs.
| Clinical Presentation | Diagnostic Tests |
|---|---|
| Dysphagia (difficulty swallowing) | Barium swallow test |
| Regurgitation of undigested food | Barium swallow test |
| Weight loss | — |
| Chest pain (occasionally) | — |
| — | Esophageal manometry |
By mixing symptoms with tests, doctors can accurately spot achalasia. Why? This guides them to the best ways to treat and manage the condition. Ultimately, this helps those with achalasia lead better lives.
Achalasia Treatment Options
There are several ways to treat achalasia. The goal is to ease symptoms, better the esophagus, and avoid problems. Here are the main options:
Lifestyle Modifications
Changing some habits can help those with achalasia. This might mean:
- Eating smaller meals more often
- Skipping foods that make symptoms worse, like spicy or greasy food
- Chewing food well and taking small bites
- Drinking lots of fluids to help swallow
Medications
Doctors might give meds to reduce issues and help the esophagus work better. Drugs often used include:
- Calcium channel blockers
- Nitrates
Endoscopic Therapies
These treatments can open up the esophagus for a while and make swallowing easier. They are:
- In balloon dilation, a balloon stretches the tight part of the esophagus.
- In botulinum toxin injection, the muscle ring gets a shot to relax for a bit.
Surgical Interventions
If lifestyle changes and medicines don’t work, surgery might be needed. The main surgery is a Heller myotomy. It cuts the esophagus muscle to let food through easier.
Stem Cell Therapy
Stem cell treatment looks at healing the esophagus. It’s new and aims to fix achalasia by repairing the affected areas. But, more study is necessary to know if it’s truly safe and effective.
It’s key to talk to your doctor about what treatment fits you best. They’ll think about how severe your achalasia is, your health, and what you hope to get from treatment. With the right care, many people see a big difference in how they feel and their life quality.
| Treatment Option | Advantages | Disadvantages |
|---|---|---|
| Lifestyle Modifications | – Easy to start – Can make you feel better overall |
– Not always enough for everyone – Need to stick with it |
| Medications | – Eases the muscle in the esophagus – Helps with swallowing |
– Might have bad effects – Doesn’t help all people |
| Endoscopic Therapies | – Not as hard on the body – Gives short relief from symptoms |
– Might need more than one treatment – Could lead to issues |
| Surgical Interventions | – Makes swallowing better for a long time – Enhances the esophagus function |
– A big surgery to go through – Carries some risks |
| Stem Cell Therapy | – Aims for the esophagus to heal itself – Could fix the problem for good |
– Still being tested – Hard to find and might not be ready |
Prognosis and Complications of Achalasia
The future for those with achalasia can look different based on their care and treatment. Most patients see their symptoms improve drastically with the right treatment. Still, there are some for whom symptoms linger despite efforts.
Prognosis of Achalasia
Life with achalasia means always managing its effects. While a cure is not available, treatments are there to ease symptoms, improve esophagus health, and stop problems before they start. Working with doctors and following lifestyle changes can keep symptoms at bay.
Creating a treatment plan with your doctor is key. This plan should match your specific condition and health goals. Regular visits for check-ups ensure any needed adjustments to the plan can be made in time.
Complications of Achalasia
Achalasia, if not managed well, can cause serious issues. These include problems like difficulty eating, lung infections, tearing in the esophagus, and a slight rise in esophageal cancer risk. Yet, the cancer risk is typically low.
Staying on top of your condition with your healthcare team is very important. Regular check-ups and tests can catch these problems early. This way, you work to avoid these complications altogether.
Good communication with your healthcare provider is vital. If your symptoms worsen or change, let them know right away. With the right approach and care, living a fulfilling life with achalasia is very possible. Your health journey should focus on well-being and quality of life.
Stem Cell Therapy for Achalasia
Stem cell therapy is a new way to treat achalasia by repairing the esophagus. Stem cells can turn into different cell types and may repair the damaged parts of the esophagus for those with achalasia. They are implanted in the esophagus to help it work properly again.
Studies show stem cell therapy might make symptoms better and improve life for those with achalasia. This method aims to place healthy cells where the esophagus is damaged. The goal is to fix the main issue of achalasia and bring long-term relief.
But, we still need more research to know if this therapy is truly safe and effective for achalasia. Many trials are testing this treatment to learn more about its benefits and risks.
Even though stem cell therapy has promise, talking to experts is crucial before considering it for achalasia. Health professionals experienced in this field can give specific advice and suggest the best treatment options for each person.
Potential Benefits of Stem Cell Therapy for Achalasia:
- Promotes repair and regeneration of damaged esophageal tissues
- Addresses the underlying cause of achalasia
- Improves esophageal function and swallowing ability
- Potential long-term relief from symptoms
Limitations and Considerations:
- Further research is needed to fully understand the effectiveness and safety
- Clinical trials are ongoing to evaluate the benefits and risks in more detail
- Treatment suitability should be determined on a case-by-case basis
- Consultation with a healthcare professional specializing in stem cell therapy is crucial
With more studies, we may better see the place of stem cell therapy in achalasia treatment. It could be a big change, offering new hope and better results for people with achalasia.
Achalasia Research and Advances
Researchers are working hard to learn more about achalasia. They’re looking for better ways to treat it. The goal is to help people with achalasia more effectively and with treatments that are right for them.
Advances in Imaging Techniques
New imaging methods are helping us understand achalasia. High-resolution manometry and impedance planimetry are key. They show us how the esophagus works, making diagnosis and planning treatment easier.
Clinical Trials for New Treatment Modalities
Right now, there are clinical trials testing new achalasia treatments. Stem cell therapy is one area being explored. It aims to repair the damaged parts of the esophagus. This could mean a big breakthrough in treating achalasia.
Along with stem cells, new drugs and treatments are being tested. The hope is to find ways to ease symptoms and improve lives for people with achalasia.
Advancing Our Knowledge and Treatment Options
All this research is promising for achalasia’s future. It’s helping us understand and treat the condition better. With these new findings, we aim to help those with achalasia have a higher quality of life.
Achalasia Management and Support
To manage achalasia well, a team of experts is needed. This includes doctors who are specialists, surgeons, and dietitians. It’s important to see these experts regularly and keep in touch. They help to watch your symptoms, change treatment if needed, and solve problems fast. This teamwork makes sure you get the right care for you.
Getting help from doctors is crucial, but support from others facing achalasia is also important. Joining support groups and using education resources can really help. You’ll meet people who understand and can share advice. Plus, you’ll find lots of helpful info and tips to handle your achalasia well.
Support groups offer a place to talk, share, and learn from each other. You can join groups either in-person or online. This way, you can meet people worldwide and get lots of useful advice. Going to these meetings can keep you informed, motivated, and strong in dealing with achalasia.
There are also many tools to help you learn more about achalasia. These include websites, materials, and forums. Learning about the condition and treatment can help you take an active role in your care.
Benefits of Achalasia Support and Education:
- Emotional Support: Talking to those who get what you’re going through can offer comfort and uplift.
- Information and Resources: Resources give you the knowledge and tips to handle achalasia better.
- Sharing Experiences: Support groups let you swap stories and advice with others in similar situations.
- Empowerment: Understanding achalasia puts you in a position to make choices and be involved in your care.
- Improved Quality of Life: With support and knowledge, your emotional well-being and overall life can get better.
Managing achalasia is a journey you’re not alone in. A strong support network and helpful resources can make a big difference. Talk to your doctors about finding local support groups and more resources. They can help you take steps to better manage achalasia and find a caring community.
Future Directions in Achalasia Treatment
Achalasia treatment is always getting better. New research and progress mean better ways to handle this condition. We are looking forward to new methods that are more focused on each person’s needs.
Stem cell therapy is a key area of study. Scientists want to use the healing power of stem cells to fix the esophagus in achalasia patients. This could bring a lasting cure, making the esophagus work better and reducing symptoms.
Another promising field is tissue engineering. It mixes biology with therapy to make new esophageal tissues. These new tissues could replace the damaged parts in achalasia. This might be a game changer, making treatment last longer than it does now.
Precise medicine is also advancing in achalasia care. This means treatments are shaped by a person’s genes, lifestyle, and condition. New research in genetics and diagnostics aims to make treatments that are just right for each achalasia patient.
Advances in Minimally Invasive Surgical Techniques
Robotic surgery and other less invasive methods are set to grow in achalasia treatment. Robotic surgery is better than open surgery because it causes less scarring and allows quicker recovery.
This method is becoming more common for achalasia surgery, which will likely lead to better results.
Advancements in Diagnostic Tools and Imaging Techniques
New diagnostic tools and imaging are also making headway. Technologies like high-resolution manometry give detailed info on the esophagus. They can help spot achalasia earlier and start treatment sooner, improving care.
In conclusion, achalasia treatment is looking up. Stem cell therapy, tissue engineering, personalized medicine, robotic surgery, and better diagnostics are on the way. These changes could make a big difference in how we treat achalasia, offering more specific and effective care options.
Conclusion
Achalasia is a rare disorder affecting the esophagus. It makes swallowing difficult and sometimes painful. This happens because the esophagus loses its ability to let food into the stomach properly.
Diagnosing achalasia includes different tests like a barium swallow and manometry. Once diagnosed, there are several ways to manage it. These include lifestyle changes, certain medications, and even surgery if needed.
Research into achalasia continues, making treatment better. People with achalasia need to stay in touch with their doctors. It’s also helpful to join support groups and educate themselves about the condition.

