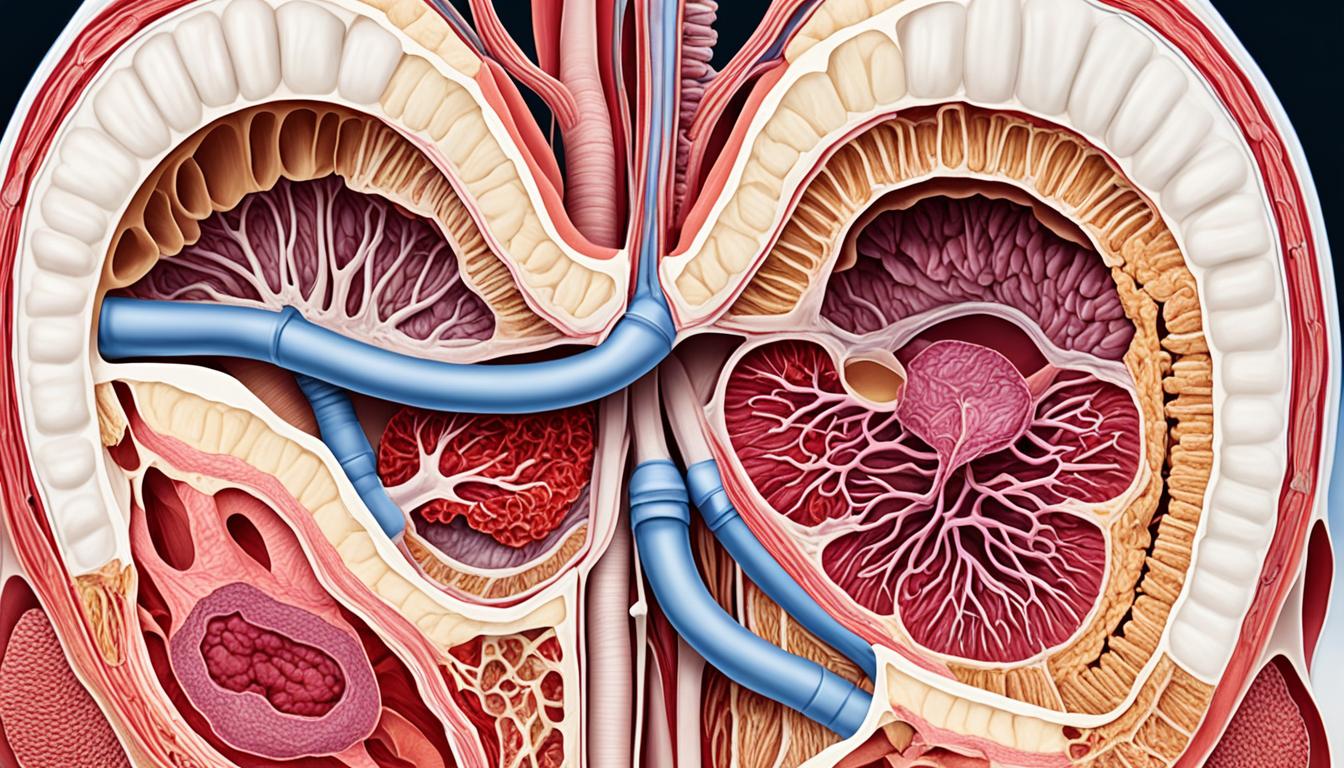
Anterior vaginal prolapse, or cystocele, is a common issue in women. It’s often seen after childbirth or as women age. It happens when the muscles that support the bladder get weak, causing the bladder to push into the vagina.
This can lead to discomfort and trouble with normal activities. Women might feel a bulge in the vagina, have trouble fully emptying their bladder, leak urine, or find sex painful. Pregnancy, aging, and obesity can increase the risk of this condition.
Doctors check for this issue through a physical exam and by talking about a woman’s health history. Treatments can range from doing special exercises for the pelvic floor to placing a device called a pessary. Surgery is also an option. But now, there’s growing excitement about using stem cell therapy to treat this condition.
Key Takeaways:
- Anterior vaginal prolapse is a common pelvic floor problem in women.
- It’s often linked to having children, getting older, and being overweight.
- Symptoms include feeling a bulge, not fully emptying your bladder, and leaking urine.
- Doctors usually diagnose it with a physical exam and by asking about a woman’s health history.
- There are several ways to treat it, like doing special exercises, surgery, and using new methods like stem cell therapy.
Prevalence and Risk Factors for Anterior Vaginal Prolapse
Anterior vaginal prolapse is a common type of pelvic organ prolapse. Many studies have looked at how often it happens and what makes it more likely. In Sweden, a study found that around 20% of women from 20 to 59 had genital prolapse, which includes anterior vaginal prolapse [1]. In the United States, 11-20% of women require surgery for prolapse during their lives [7]. This shows how big of an issue anterior vaginal prolapse is as a problem with the pelvic floor.
Several things can make anterior vaginal prolapse more likely. Giving birth vaginally is a major risk factor [7]. It weakens the pelvic floor muscles. This makes it easier for the pelvic organs to fall out of place. Getting older and being overweight also raise the risk [7, 16]. Changes in hormones and more pressure on the pelvic area are often seen in these situations. Some people might be more likely to get anterior vaginal prolapse because of their genes [26]. Other things that could lead to it are diseases affecting connective tissue, long-term constipation, and lifting heavy things often [7, 16, 26].
Prevalence of Anterior Vaginal Prolapse:
- A study in Sweden found the prevalence of genital prolapse, including anterior vaginal prolapse, to be around 20% among women between the ages of 20 and 59 [1].
- In the United States, 11-20% of women undergo surgery for prolapse in their lifetime [7].
Risk Factors for Anterior Vaginal Prolapse:
- Childbirth, especially through vaginal delivery, increases the risk of anterior vaginal prolapse [7].
- Advanced age and obesity are associated with a higher risk of developing anterior vaginal prolapse [7, 16].
- There may be a genetic predisposition to pelvic organ prolapse [26].
- Connective tissue disorders, chronic constipation, and repetitive heavy lifting have also been identified as contributing factors [7, 16, 26].
Symptoms of Anterior Vaginal Prolapse
Anterior vaginal prolapse is also known as cystocele. It has different symptoms of varying severity. Learning these symptoms is crucial to get the right medical help.
Symptoms include:
- A bulging or protrusion in the vagina
- A feeling of heaviness or pressure in the pelvic area
- Difficulty emptying the bladder completely
- Urinary incontinence
- Discomfort or pain during sexual intercourse
- Lower back pain
- Recurrent urinary tract infections
The signs range from mild to severe. They can get worse with actions that push on the abdomen. This includes coughing, sneezing, or lifting heavy things. Yet, not every woman with this issue has the same symptoms. And the seriousness of these symptoms varies from one person to another.
If you notice any of these signs, it’s best to see a doctor. They can provide the right diagnosis and treatment. Getting help early can reduce symptoms and enhance your life.
| Symptoms | Prevalence |
|---|---|
| Bulging or protrusion in the vagina | 82% |
| Feeling of heaviness or pressure in the pelvic area | 78% |
| Difficulty emptying the bladder completely | 64% |
| Urinary incontinence | 57% |
| Discomfort or pain during sexual intercourse | 49% |
| Lower back pain | 36% |
| Recurrent urinary tract infections | 28% |
Diagnosis of Anterior Vaginal Prolapse
Diagnosing anterior vaginal prolapse starts with a detailed check-up. [3] The doctor checks the support and position of the pelvic organs by looking at the vagina. They may also ask the patient to push down, like when using the bathroom.
Sometimes, more tests are needed. These could include urodynamic studies, where how well the bladder works is checked. Or imaging tests, like ultrasound or MRI, to see the prolapse clearly and understand its severity. These tests help identify any risks or complications from the prolapse.
Seeing a healthcare professional is crucial for the right diagnosis and treatment plan. The doctor will look at the patient’s symptoms, health history, and exam results to properly diagnose. They also take the patient’s overall health and lifestyle into consideration for planning the treatment.
It’s important to visit a doctor who specializes in pelvic floor issues for a reliable diagnosis. This leads to a treatment plan that’s right for the patient’s specific situation.
Treatment Options for Anterior Vaginal Prolapse
The way we treat anterior vaginal prolapse depends on how bad it is and the effect on a person’s life. For mild to moderate cases, your doctor might suggest doing Kegel exercises or using pessaries. Pessaries are devices placed in the vagina to hold up the organs. For more serious cases or when these methods don’t work, surgery might be needed.
When it comes to surgery, there are a few options. This includes fixing the vaginal wall, sometimes taking out the uterus, and using either man-made or natural mesh to help the organs. By fixing the vaginal wall, doctors can move and secure the weak tissues and muscles. Hysterectomy can help if the uterus is part of the problem. Lab-made or natural mesh provides strong support for a long time.
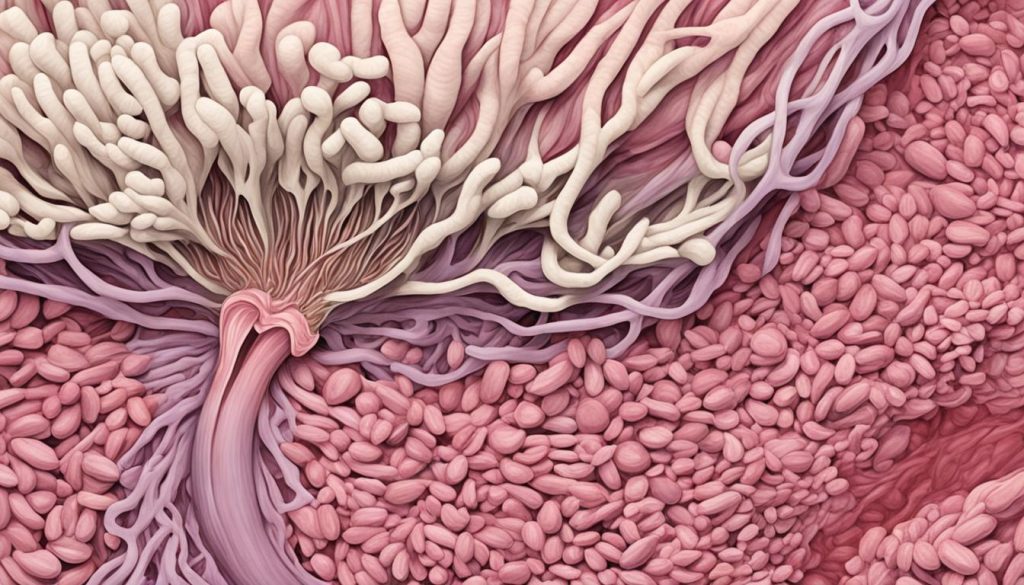
Now, there’s another treatment being looked into: stem cell therapy. Early research shows it could help a lot. Stem cells help new tissue grow and repair. This can make the pelvic organs stronger. Scientists are trying stem cells from places like fat and bone marrow to see if they can heal the pelvic floor better.
| Treatment Options | Description |
|---|---|
| Pelvic Floor Exercises (Kegel exercises) | Specific exercises that target and strengthen the muscles of the pelvic floor, improving support for the pelvic organs. |
| Pessaries | Medical devices that are inserted into the vagina to provide support to the pelvic organs. |
| Vaginal Wall Repair | Surgical procedure to reposition and secure the weakened tissues and muscles of the vaginal wall. |
| Hysterectomy | Surgical removal of the uterus, which may be recommended if the uterus is contributing to the prolapse. |
| Synthetic or Biological Mesh | Use of mesh materials to reinforce weakened tissues and provide additional support to the pelvic organs. |
| Stem Cell Therapy | Experimental approach involving the use of stem cells to promote tissue regeneration and repair in the pelvic floor. |
Complications and Long-Term Outlook for Anterior Vaginal Prolapse
Anterior vaginal prolapse is a condition that needs treatment. If ignored, it can lower a woman’s life quality. Complications may lead to recurring urinary tract infections, urine leaks, and trouble during sex. These issues can cause stress. The long-term picture for this condition varies. It depends on its seriousness, the treatment’s success, and the patient’s health and habits.
But, with the right care, many women can manage the symptoms. They can have a good quality of life.
Complications of Anterior Vaginal Prolapse
Anterior vaginal prolapse may bring several challenges. It can make getting urinary tract infections often a problem. This happens when the bladder blocks normal urine release. This could cause more UTIs. And, women may experience urine leaks, known as incontinence. This is because the condition weakens the body’s pelvic floor and shifts organs. Problems during sex may also happen. This makes sex uncomfortable and painful. It might reduce sexual desire and intimacy. The situation can also bring emotional stress and affect life quality. So, seeking help is key to avoid or manage these effects.
Long-Term Outlook for Anterior Vaginal Prolapse
The long-term impact of anterior vaginal prolapse varies. It depends on the prolapse’s seriousness, how well treatment works, and a person’s health and habits. Good care helps many women manage their symptoms well and lead a good life.
Things like exercises and pessaries can help. Surgery might be needed in severe cases. It is vital for women to closely work with their doctors. This ensures the right treatment. They should also get regular check-ups to watch for any new issues or changes. This care is crucial [9, 14].
Getting the right treatment in time improves symptoms and the long-term outcome. This makes sure women enjoy a better life and health.
Research and Advancements in Anterior Vaginal Prolapse
Scientists are working to learn more about anterior vaginal prolapse. They want to know what causes it and how to treat it. They study things like genes, hormones, and muscle health [16, 19, 26].
New technology has also helped. For example, single-cell RNA sequencing. This technology gives us a closer look at what happens on a cell and molecular level in ovaries [2, 12, 20].
There is hope in stem cell therapy for this issue. Studies have shown positive signs. But we still need more research to be sure about its safety and how well it works long-term [23, 31].
Current Research Areas:
- Genetics: Looking into what genetic parts might make a person more likely to get anterior vaginal prolapse.
- Hormonal Factors: Seeing how hormonal changes might weaken the body’s support for the organs.
- Muscle Function: Checking how muscle problems can make pelvic organs less stable.
- Single-Cell RNA Sequencing: Figuring out the inside changes in cells that could lead to the problem.
- Stem Cell Therapy: Looking at if stem cells can help repair the damaged areas.
Progress in researching anterior vaginal prolapse is encouraging. It brings hope of finding better ways to understand and treat it. This may benefit many women with the condition.
Lifestyle and Self-Care Tips for Anterior Vaginal Prolapse
Aside from medical help, lifestyle changes and self-care can ease anterior vaginal prolapse symptoms. Adding these to your daily life helps a lot. It makes you feel better and reduces the pain.
Maintain a Healthy Lifestyle
Staying at a healthy weight is key. Too much weight stresses your pelvis and makes symptoms worse. Eat a lot of fruits, veggies, whole grains, and lean meats. This keeps your weight in check and boosts your health.
Practice Good Posture
Having good posture helps your pelvic organs stay where they should. Stand and sit straight to ease the pressure. Exercises that make your core and back stronger also help a lot.
Avoid Heavy Lifting
Lifting heavy things strains your pelvic floor and makes prolapse symptoms worse. Limit activities that require heavy lifting. Always use the right form when you lift, bending your legs and not your back.
Manage Chronic Constipation
Constipation can make anterior vaginal prolapse symptoms worse. Eat foods rich in fiber, drink plenty of water, and stay active to avoid it. Talk to a doctor if you need extra help with this.
Pelvic Floor Exercises
Kegel exercises are great for strengthening the pelvic floor. Doing them often can help ease symptoms and stop prolapse from getting worse. A health expert can show you the best way to do these exercises.
Every woman’s prolapse is different. What helps one may not help another. Seeing a specialist in pelvic floor disorders can guide you in the best care. Use these tips along with your medical treatment to better your life.
Conclusion
Anterior vaginal prolapse, or vaginal wall prolapse, is common among women, especially after childbirth or with age. It can cause mild to severe symptoms. Luckily, there are many ways to treat it, from simple steps to surgeries and even new treatments like stem cell therapy.
The right treatment depends on a person’s situation and what they prefer. It’s key to get diagnosed quickly and start treatment. This can ease symptoms and make life better. As we learn more, there is hope for even better treatments in the future.
If you know someone with anterior vaginal prolapse or think you might have it, it’s important to see a doctor. With proper care, women can handle this condition well. They can get back to feeling comfortable and confident.
FAQ
Q: What is anterior vaginal prolapse?
A: Anterior vaginal prolapse happens when the bladder bulges into the vagina. This happens because of weak tissues and muscles. They can’t support the bladder well.
Q: What are the symptoms of anterior vaginal prolapse?
A: The symptoms include feeling a bulge in the vagina and having trouble with the bladder. You might leak urine, feel pain during sex, or have a heavy feeling in your pelvic area.
Q: How is anterior vaginal prolapse diagnosed?
A: Doctors do a physical check to find out if you have anterior vaginal prolapse. They look at how well your pelvic organs are supported. Sometimes, they might need more tests like a urodynamic study or imaging.
Q: What are the treatment options for anterior vaginal prolapse?
A: To treat this, you might do pelvic exercises or use pessaries. For severe cases, surgery could help. There’s also hope in stem cell therapy.
Q: What are the complications and long-term outlook for anterior vaginal prolapse?
A: Complications can be urinary problems, pain with sex, or feeling down. The long-term outcome is different for each person. It depends on how bad the prolapse is and how well the treatment works.
Q: What research and advancements are being made in the field of anterior vaginal prolapse?
A: Researchers are looking for better ways to treat this condition. They study its causes, how treatment works, and new options like stem cell therapy. Advancements in technology are helping too.
Q: What lifestyle and self-care tips can help manage anterior vaginal prolapse?
A: To help with this condition, you should keep fit and stand straight. Don’t lift heavy things. Also, avoid constipation and do pelvic exercises.