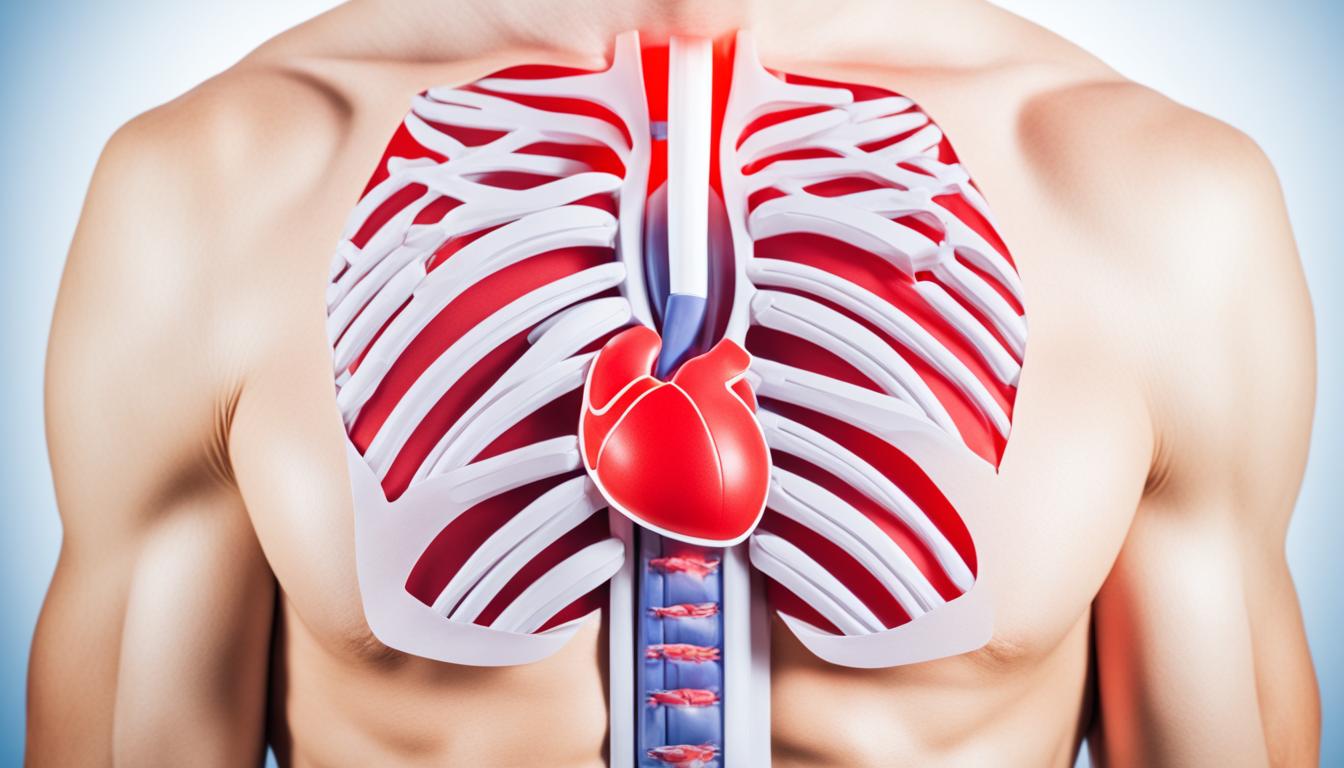
Angina pectoris is a heart condition that brings chest pain, tightness, and pressure. Knowing the symptoms, causes, and how it’s diagnosed is key to fighting it. Early treatment is crucial to stop it from turning into a heart attack.
Many things can lead to angina pectoris, like smoking, high blood pressure, and not being active. By being aware of these risks, people can lower their chances of getting it.
Doctors diagnosis angina through several tests and checks. This can involve looking at your heart history and using tools like ECG tests. A full check-up helps them find the best way to treat you.
Recently, stem cell therapy has shown promise in treating angina pectoris. It’s all about using cells to fix the heart’s issues. Research is optimistic about how this could help people live better.
Key Takeaways:
- Angina pectoris is characterized by chest pain, tightness, and pressure.
- Risk factors for angina pectoris include smoking, high blood pressure, high cholesterol levels, obesity, and a sedentary lifestyle.
- Diagnosis involves a comprehensive examination and diagnostic tests like ECG and angiography.
- Stem cell therapy shows promise in regenerating damaged heart tissues and improving heart function.
- Prompt treatment and lifestyle modifications are crucial for managing angina pectoris and preventing complications.
Types of Angina Pectoris
Angina pectoris is a key sign of heart problems, showing up in three main types. These are atypical, unstable, and exertional angina.
Atypical Angina (Coronary Angina)
Atypical angina or coronary spastic angina is one form. It happens when the smooth muscles in the arteries suddenly tighten. This can block blood flow to the heart, causing pain.
Unstable Angina
Unstable angina is very serious. It’s often due to blood clots in the arteries. If not treated quickly, it can lead to a heart attack.
Exertional Angina
Exertional angina shows up during activities or exercise. Not enough oxygen can get to the heart, causing pain. But it fades away with rest.
To better understand the differences in angina types, check out this table:
| Type of Angina | Description |
|---|---|
| Atypical Angina | Characterized by temporary spasms or narrowing of coronary arteries |
| Unstable Angina | Caused by blood clots blocking the coronary arteries |
| Exertional Angina | Occurs during physical activity and is relieved by rest |
Myocardial Infarction
Myocardial infarction, or heart attack, is a main cause of death. It happens when a blood clot stops a heart vessel. This leads to heart damage. It can slow movement and affect whole-body blood flow. Signs include severe chest pain that lasts more than 20 minutes, even at rest. Quick treatment is crucial to avoid cardiac arrest and other serious issues.
Difference Between Angina Pectoris and Myocardial Infarction
It’s key to know the difference between angina pectoris and myocardial infarction in heart health. Both can bring on chest pain yet work differently.
Angina Pectoris
Angina pectoris is a sign that your heart’s blood vessels are narrowing. This leads to less blood reaching the heart. You might feel chest pain, discomfort, or pressure. Even with this issue, your heart’s function is usually not harmed.
Myocardial Infarction
Myocardial infarction, or a heart attack, happens when the heart’s blood flow is fully blocked. A blood clot often causes this blockage. The heart muscle doesn’t get the oxygen and nutrients it needs, causing serious harm. Without care, a heart attack can lead to severe problems or death. This is a stark difference from angina pectoris because the blood flow is entirely cut off.
Sometimes, angina pectoris can lead to a heart attack if not treated quickly. Seeking medical help promptly for angina is essential to avoid this situation.
Generally speaking, angina pectoris and myocardial infarction both affect the heart’s blood flow and can cause chest pain. But angina involves a partial blood flow block, unlike the full block in a heart attack. The former doesn’t damage the heart long-term as a heart attack can.
| Angina Pectoris | Myocardial Infarction |
|---|---|
| Temporary narrowing of coronary arteries | Complete blockage of coronary arteries |
| Reduced blood flow to the heart | Deprived blood flow to the heart |
| Preserved heart function | Heart dysfunction and potential cardiac arrest |
Treatment Options for Angina Pectoris and Myocardial Infarction
Quick treatment is key for angina pectoris and myocardial infarction. Several treatments help manage these and boost patient endings. The right one depends on disease severity and the patient’s medical story.
1. Drug Therapy
Using medicines is a usual way to handle angina pectoris. These work to ease symptoms and stop more episodes. They also lower the risk of a heart attack. Nitroglycerin and beta-blockers are often used. Nitroglycerin opens heart arteries to boost blood flow. Beta-blockers ease the heart’s job and help with blood pressure.
2. Catheter Therapy
Procedures with a catheter, like PCI, can treat unstable angina and heart attacks. In PCI, a balloon-tipped catheter goes into the blocked artery. The balloon opens the artery by pushing plaque out of the way. Stents, which are tiny tubes, can also help keep the artery open and smooth out blood flow.
3. Surgical Therapy
For severe artery blockages, surgery might be needed. CABG is a common surgery. It creates a new path around the blocked parts using a vein from elsewhere on the body. This lets blood reach the heart better, easing symptoms, and cutting heart attack risks.
4. Regenerative Medicine
Regenerative approaches like stem cells could be very helpful. They might fix damaged heart tissue and improve how the heart works. This method looks into jumpstarting the heart’s self-healing and making life better for the patients. Scientists are hard at work to make sure this treatment is safe and works well.
The image above shows all available treatments for angina and heart attacks. It’s all about easing symptoms, improving blood flow, and stopping more issues. Always talk to a doctor to pick what’s best for you.
Causes and Prevention Methods of Angina and Myocardial Infarction
Lifestyle choices play a big role in angina pectoris and myocardial infarction. Many factors can lead to these heart diseases, like smoking, being overweight, not exercising enough, stress, and getting older. You can lower your risk of getting these diseases by changing your lifestyle. This means eating right, regular exercise, and learning to manage stress properly.
Arteriosclerosis: The Underlying Cause
The main reason why angina and heart attacks happen is arteriosclerosis. This happens when your arteries become hard and narrow because of plaque buildup. As the arteries get narrower, blood flow to your heart is reduced. This can lead to chest pain and a higher chance of a heart attack. Luckily, arteriosclerosis can be prevented by making healthier life choices.
Preventing Angina and Myocardial Infarction
Stopping these heart diseases before they start is the best approach. Here’s how:
- Adopt a Healthy Diet: Eat less saturated fats, cholesterol, and sodium, and more fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Engage in Regular Exercise: Do activities that make your heart beat faster. This helps keep a healthy weight, lowers blood pressure, and boosts heart health. Aim for 150 minutes of moderate exercise or 75 minutes of intense exercise each week.
- Manage Stress: Deal with stress in healthy ways, like meditation, hobbies, or talking with family and friends.
- Avoid Smoking: Smoking harms blood vessels, raises clotting risks, and fast-tracks arteriosclerosis. Quitting is a big step for a healthier heart.
- Maintain a Healthy Weight: Extra weight is a major heart disease risk. Keeping a healthy weight cuts your angina and heart attack risks.
Taking these steps and changing your lifestyle can lower your chance of angina pectoris and myocardial infarction. Remember, even small changes can greatly improve your heart health.
Summary: Importance of Correct Eating and Lifestyle Habits
Heart diseases like angina pectoris and myocardial infarction are very serious and can be deadly. Though we have many treatments, it’s better to avoid these diseases if we can. They often show no symptoms and can hit hard. So, fixing how we eat and live is key to keeping our hearts strong. By being mindful of our daily choices, we lower the risk of heart issues.
The Impact of Lifestyle Habits on Heart Health
Our heart’s health links closely to how we live. Bad eating, no exercise, smoking, and too much stress up our heart disease risk. But switching to good habits can cut the chance of heart troubles.
Eating Habits for Heart Health
A diet that’s good for the heart fights off these diseases. Fill up on fruits, veggies, whole grains, lean meats, and good fats to keep your blood flowing. But remember, too much bad fats and salt can hurt your heart.
Physical Activity and Exercise
Staying active keeps heart problems away. Do things like walking, swimming, or biking for 150 minutes each week to boost your heart’s health. It helps you stay fit, lowers blood pressure, and makes your heart work better, which protects it from diseases.
Stress Management and Mental Health
Stress is bad news for your heart. It can cause inflammation and raise your risk of diseases. A calm mind and happy heart go together. So, try relaxation, mindfulness, and lean on your loved ones for support to keep stress low.
The Role of Smoking and Alcohol Consumption
Smoking and too much alcohol are big no-nos for heart health. Cutting back on these dramatically cuts your chance of getting sick. Smoking messes with your blood vessels and alcohol can damage your heart’s rhythm and muscle.
Regular Check-ups and Early Detection
Seeing your doctor often helps catch heart problems early. Tests like blood pressure checks, cholesterol tests, and ECGs can show if you’re at risk. An early start to fixing things can really save your heart in the long run.
Choosing good food, keeping active, and watching stress can do wonders for your heart. If you skip smoking and watch how much you drink, you’re adding more years to your life. It sets you on a path to avoid heart problems early on.
| Heart-Healthy Eating Habits | Recommended Frequency |
|---|---|
| Consume a variety of fruits and vegetables | Every day |
| Incorporate whole grains into meals | Every day |
| Choose lean sources of protein | Regularly |
| Include healthy fats, such as avocados and nuts | In moderation |
| Limit saturated fats and trans fats | Sparingly |
| Reduce sodium intake | Minimize |
| Avoid sugary beverages and excess added sugars | Sparingly |
Diagnosis and Management Guidelines for Chronic Coronary Syndromes
Finding the problem and how to take care of it is key in helping people with chronic coronary syndromes. The 2019 ESC guidelines give doctors and nurses clear steps to follow. These help in making sure everyone gets the best care possible.
Diagnosis:
Finding the right treatment starts with a precise diagnosis. Doctors look at many things like age, gender, and family history. They may do tests like stress tests and echocardiograms to understand the heart better. These help find any blockages or issues right away.
Management Guidelines:
Once the doctor knows what’s going on, they plan how to help. The treatment changes from person to person. It often involves medicines, some procedures with thin tubes, or even surgery. The decision is based on the patient’s specific situation and how serious it is.
Drug Therapy:
Drugs are a big part of treating chronic coronary syndromes. Heart medicines like beta-blockers and ACE inhibitors are often used. They help lessen symptoms, keep blood from clotting, and control blood pressure and cholesterol.
Catheter Therapy:
Some treatments happen without surgery. One common way is through a heart catheter. Doctors place a small tube with a balloon or stent in the artery to open it. This helps blood flow better to the heart.
Surgical Therapy:
When other methods aren’t enough, surgery might be the answer. Coronary bypass surgery is one type. A bypass allows blood to travel around a blocked artery. This lets the heart get the blood it needs to stay healthy.
The care for each person is unique when it comes to chronic coronary syndromes. Doctors and patients work together to choose what’s best. This approach leads to better care and a higher quality of life for those with this condition.
| Treatment Options | Description |
|---|---|
| Drug Therapy | Combination of medications to manage symptoms and reduce the risk of complications. |
| Catheter Therapy | Minimally invasive procedures to open up blocked or narrowed coronary arteries. |
| Surgical Therapy | Invasive procedures, such as coronary artery bypass grafting (CABG), to bypass blocked arteries. |
Current Research and Advancements in Angina Pectoris and Myocardial Infarction
Over time, as research grows, so does our knowledge and ways to treat angina pectoris and myocardial infarction. New approaches are being looked into to help patients with heart issues.
One key area is looking at special medicines for these conditions. These drugs target the root of the illnesses and aim to treat them better. Improving how we treat these conditions is a major goal.
Regenerative medicine, like stem cell therapy, shows a lot of promise too. It can help the heart work better and heal damaged tissue. Research is looking into how safe and effective this therapy is, offering a bright future for heart health.
There’s also progress in heart procedures that are less risky and more effective. Things like percutaneous coronary intervention and using stents are getting better each day. This means a brighter future for those with heart problems.

Exploring New Frontiers: Current Studies and Trials
Studies and trials are pushing the boundaries in heart research every day. They aim to find new treatments, look into new technologies, and find big breakthroughs. These could change how we manage heart conditions.
Researchers are testing new drugs, new procedures, and new ways to diagnose heart problems. They’re also looking at how genetic and molecular therapies can offer personalized care. Combining all these efforts gives doctors a deeper knowledge to provide the best care.
So, ongoing studies are making a big difference in heart care. They’re bringing in new therapies and techniques, giving hope for better health. As science progresses, we’re getting closer to improving how we treat and manage heart issues.
Conclusion
Managing angina pectoris and stopping it from becoming a heart attack is key. Start by living healthily. This means eating well, staying active, and keeping stress low. This helps lower the chances of heart issues.
Angina and heart attacks are very serious if not treated. Yet, there are ways to keep them in check. Early care and healthy living are vital. This lets you live fully without being held back by these heart problems.
Focus on your heart early with lifestyle changes and good medical help. Remember, these heart issues can be kept under control. A heart-smart life is essential for a healthy heart. With these efforts, you can cut your risk and live more fully.
FAQ
Q: What are the symptoms of angina pectoris?
A: Symptoms of angina pectoris are chest pain, tightness, and pressure. These can happen when not enough blood reaches the heart.
Q: What are the types of angina pectoris?
A: There are three types: atypical, unstable, and exertional angina. Each has its own set of triggers and symptoms.
Q: What is the difference between angina pectoris and myocardial infarction?
A: Angina is caused by temporary blockages in blood flow to the heart. A heart attack, or myocardial infarction, is when a blockage is full and lasting.
Q: What are the treatment options for angina pectoris and myocardial infarction?
A: Treatments may vary. They can include medications, procedures like stents, surgery, or newer methods like regenerative medicine.
Q: What are the causes and prevention methods of angina and myocardial infarction?
A: Causes are often related to unhealthy lifestyles or aging. These include smoking, not exercising, stress, and being overweight.
Preventing these heart issues involves a balanced diet, staying active, and managing stress better.
Q: What are the diagnosis and management guidelines for chronic coronary syndromes?
A: The 2019 guidelines talk about how to find the risks and the best ways to treat. They suggest tests and personalized care for patients.
Q: What are the current research and advancements in angina pectoris and myocardial infarction?
A: New studies focus on better therapies, ways to heal the heart, and advanced heart procedures. This aims to improve patient outcomes.