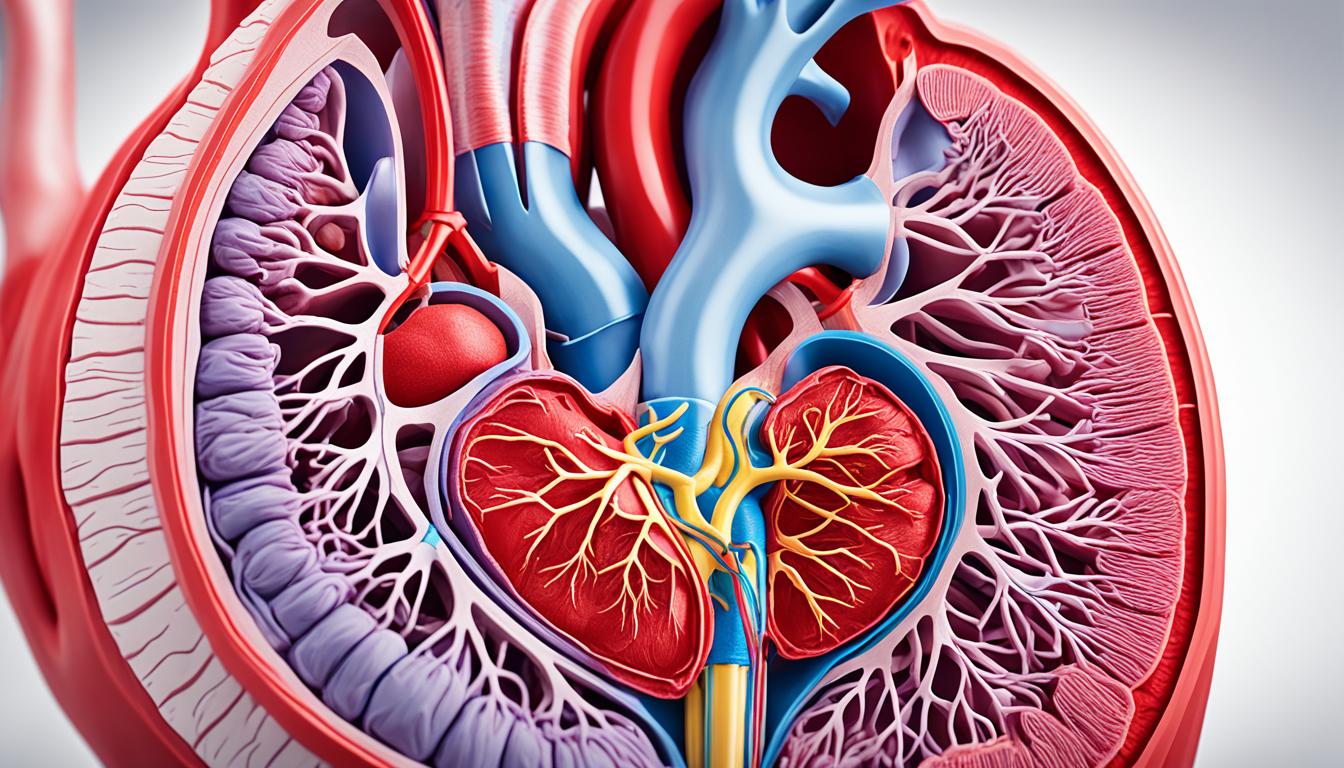
Patent foramen ovale (PFO) is a heart defect at birth. It shows a hole in the wall between the heart’s upper chambers. Normally, this hole closes soon after a person is born. But 25% of adults may still have it open. This open space can lead to a stroke. A clot can pass through this hole and harm the brain. The exact reason why PFO happens is not clear. It could be due to the wall not fully closing while a baby is still growing in the womb.
Diagnosing PFO is done with an echocardiogram. This test uses sound waves to see into the heart. Doctors might also do a bubble test to check for the PFO hole. Treatment for PFO includes taking blood thinners like aspirin. Or, a doctor can close the hole with a special device placed through the skin. Another option is using stem cells to try and repair the heart’s damaged tissue.
Key Takeaways:
- Patent foramen ovale (PFO) is a congenital heart defect characterized by a persistent opening in the interatrial septum.
- PFO can be responsible for cryptogenic strokes, where a blood clot passes through the PFO, causing a stroke.
- Diagnosis involves echocardiogram and additional tests to confirm the presence of PFO.
- Treatment options for PFO include medical therapy, percutaneous PFO closure, and stem cell therapy.
- Stem cell therapy has the potential to repair and regenerate the heart tissue affected by PFO.
Percutaneous PFO Closure – Controversies and Trials
Doctors have debated percutaneous PFO closure, especially in the U.S. They often suggest using aspirin or warfarin first for those with a PFO and a past cryptogenic stroke. Yet, for people who still have strokes even with the best medicine, they might consider PFO closure.
In some studies, using STARFlex or Amplatzer Multi-Fenestrated Septal Occluder devices alone was better at preventing strokes when compared to just taking medicine. But, when they compared PFO closure to medicine directly in trials like Closure I, PC, and Respect, the results were mixed.
Closure I showed no big difference in stroke or TIA rates between those who had their PFO closed and those who took medicine. The PC trial also couldn’t clearly prove PFO closure’s benefits. But, the Respect trial hinted that selecting patients based on detailed clinical and imaging results might lead to better closure outcomes.
The debates and mixed trial results suggest more studies are needed. These are crucial to figure out the best way to treat patients with a PFO.
Summary of Randomized Trials:
| Trial | Outcome |
|---|---|
| Closure I trial | No significant difference in stroke or TIA rates between closure and medical therapy groups |
| PC trial | No clear benefit of percutaneous PFO closure |
| Respect trial | Potential benefit of closure in carefully selected patients |
PFO Closure Procedure and Potential Risks
The percutaneous PFO closure procedure is a minimally invasive, catheter-based method. It involves entering the PFO through the groin’s blood vessels. A specialized device, known as an “occluder,” closes the PFO opening in the heart’s septum. This method shows good results in lowering stroke risks for some patients.
Yet, this procedure has its risks just like any other medical treatment. Serious risks include the device moving, bleeding, stroke, and infection. It’s also possible for the heart muscle to gather fluid, which might need more treatment. Other risks are blockages in blood vessels, allergies, arm or lower neck nerve damage, and the potential for needing a pacemaker.
Before doing the PFO closure, it’s key to talk with your doctor in depth. The doctor should explain all the risks and benefits of the procedure.
Patients need to realize that careful watching and follow-up are crucial after the PFO is closed. This is to check the procedure’s success and to spot any complications early.
FAQ
Q: What is patent foramen ovale (PFO)?
A: Patent foramen ovale (PFO) is a heart defect you’re born with. It makes a small hole stay open in the wall between two heart chambers.
Q: What are the symptoms of PFO?
A: Most people with PFO don’t feel sick. But, sometimes it can cause tiredness, difficulty breathing, or feeling your heart beat fast.
Q: How is PFO diagnosed?
A: An echocardiogram can show if you have PFO. This test uses sound waves to take pictures of your heart. Doctors might also do a bubble test to be sure.
Q: What are the treatment options for PFO?
A: Options include taking aspirin or a blood thinner to lower stroke risk. Another choice is a special heart device for PFO closure.
Q: What is percutaneous PFO closure?
A: It’s a surgery using a catheter that goes through a vein from the groin to your heart. A small device closes the hole in your heart.
Q: What are the potential risks of PFO closure?
A: Closing the PFO might lead to serious issues like death or stroke. It could also cause fluid around the heart, clots, or heart rhythm problems.
Less common risks are blockages, allergic reactions, and infections. Bleeding, nerve injury, needing a pacemaker, and the device moving are also possible problems.
Q: Is PFO closure effective in preventing strokes?
A: Research shows it can lower the chance of another stroke in some people. But, more studies are needed. The best way to treat PFO isn’t clear yet.
Q: What is stem cell therapy for PFO?
A: It’s a new treatment that might fix heart tissue hurt by PFO. But, we still need more research to know if it works well and is safe.
Q: What controversies and trials are associated with percutaneous PFO closure?
A: Doctors’ opinions differ, especially in the US, about this surgery. Studies like the Closure I and Respect trials give mixed answers, leading to debate.
Q: What are the potential outcomes of PFO closure?
A: Some early studies suggest PFO closure might be better than just medicine in preventing strokes. But, more research is critical to know its real benefits.
Q: Why might a patient consider PFO closure?
A: Those who keep having strokes despite medicine might look at PFO closure. It’s important to discuss this with a doctor, weighing both risks and benefits.