Hereditary nonpolyposis colorectal cancer syndrome (HNPCC), also called Lynch syndrome, is linked to a higher cancer risk. It comes from gene mutations connected to repairing DNA errors. People with HNPCC have a greater chance of getting several cancer types. This includes colorectal, endometrial, gastric cancer, and more. It affects around 1 in 300 people. HNPCC is among the common inherited cancer syndromes.
It’s important for those with a history of HNPCC-related cancers to get genetic testing. This is especially true if these cancers showed up at a young age. The test finds gene mutations and checks the risk for getting colorectal cancer. Genetic counseling for colorectal cancer is key. It gives info and helps with healthcare choices.
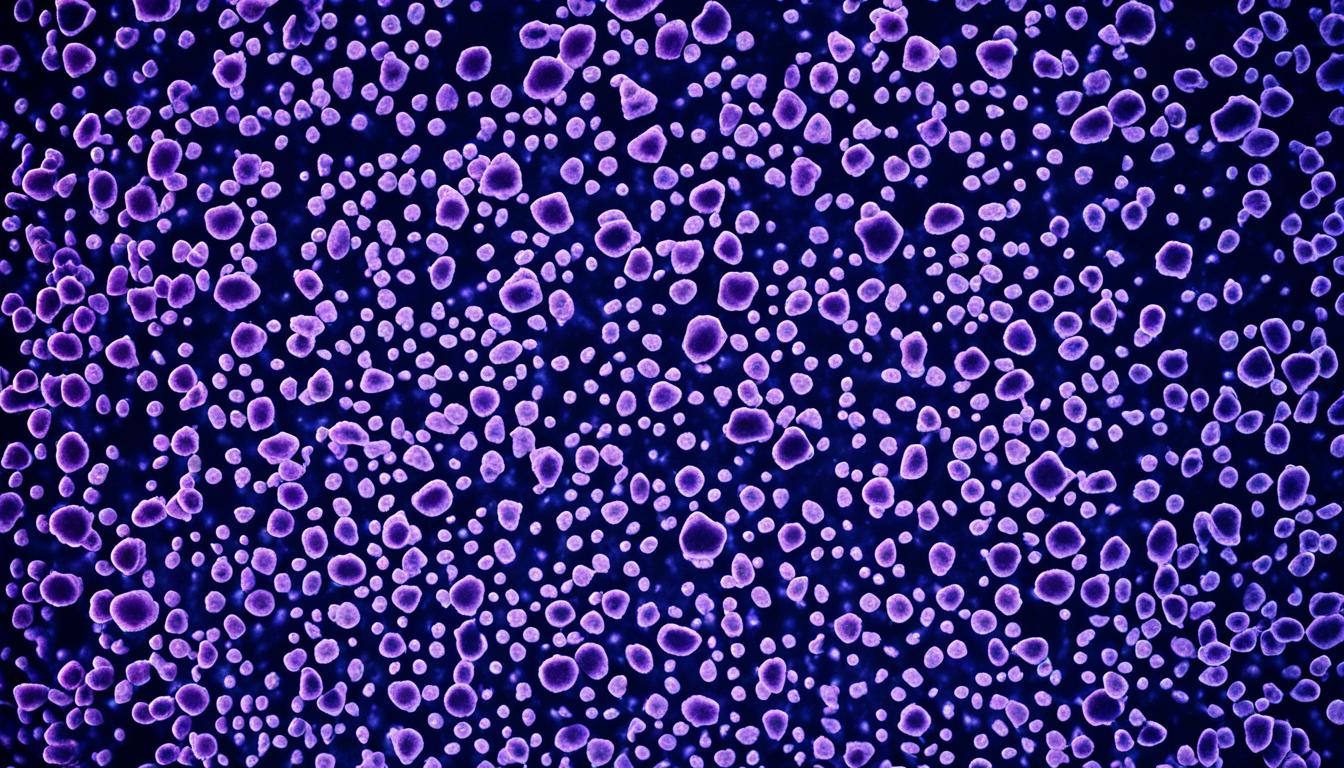
Stem cell therapy has caught interest as a possible HNPCC treatment. However, more study is necessary to check how well it works.
- Hereditary nonpolyposis colorectal cancer syndrome (HNPCC), or Lynch syndrome, raises the risk of getting various cancers.
- Malfunctions in genes that manage DNA repair cause HNPCC.
- Getting genetic testing can pinpoint gene errors and figure out the risk for colorectal cancer.
- Colorectal cancer genetic counseling equips individuals and families with crucial facts about HNPCC.
- Stem cell therapy is under study for treating HNPCC.
Signs and Diagnosis of Hereditary nonpolyposis colorectal cancer syndrome
Lynch syndrome, also called Hereditary nonpolyposis colorectal cancer syndrome, has some key signs. It’s diagnosed following the Revised Bethesda guidelines. These help doctors spot people who might have Lynch syndrome and need more tests.
If someone has colorectal or endometrial cancer before they turn 50, Lynch syndrome is a possible cause. Cancer at a young age suggests the need for Lynch syndrome testing.
Tests like microsatellite instability look for changes in the DNA of the cancer’s tissue. They check for markers that point to Lynch syndrome. Another test, immunohistochemistry, studies how proteins work, which can give clues about Lynch syndrome too.
If several family members have had these cancers, it could mean a higher Lynch syndrome risk. Family history plays a big role in diagnosis.
Getting a genetic test can confirm Lynch syndrome. It checks for changes in genes linked to Lynch syndrome. These include MLH1, MSH2, MSH6, PMS2, and EPCAM. The test tells how likely someone is to develop related cancers.
If Lynch syndrome seems possible in your family, seeing a genetics expert is important. They can organize tests and give advice on what to do next.
Revised Bethesda guidelines
The guidelines for spotting Lynch syndrome look at age when cancer starts, DNA changes, and family history. Doctors use these, plus tests like those for DNA instability, to make a diagnosis.
Microsatellite instability testing
Testing for DNA instability, by looking at special markers, helps check for Lynch syndrome. If the markers are abnormal, it could mean Lynch syndrome is more likely. This test is often done on cancer tissue.
Immunohistochemistry testing
Another test checks how certain proteins work. Issues in these proteins can show a risk for Lynch syndrome. Like the DNA test, this is done on tumor tissue as well.
Using the signs and tests for Lynch syndrome, doctors can diagnose it accurately. Finding it early is vital for the right treatment and lowering cancer risks.
Causes and Inheritance of Hereditary nonpolyposis colorectal cancer syndrome
Hereditary nonpolyposis colorectal cancer syndrome is a genetic condition. It may come from inherited mutations or ones that form in a person’s life. They affect specific genes in DNA repair. These mutations can either come from a person’s parents or show up during their life.
Inherited mutations, called germline mutations, cause about 3% of colorectal cancer. And they lead to 2% to 3% of endometrial cancer cases. These mutations happen in genes like MLH1 and MSH2. When these genes change, the chance of getting certain cancers rises.
Lynch syndrome carries an autosomal dominant inheritance pattern. This means just one mutated copy of a gene from either parent can raise disease risk. If one parent has the mutation, their child has a 50% chance of getting it, too.
Today, we can check for these mutations through genetic testing. Tests look at genes like MLH1 and MSH6, among others. This test can reveal someone’s risk of inherited cancer.
Genes Associated with Hereditary nonpolyposis colorectal cancer syndrome
| Gene | Description |
|---|---|
| MLH1 | Plays a role in DNA mismatch repair |
| MSH2 | Involved in DNA mismatch repair processes |
| MSH6 | Plays a role in maintaining genomic stability |
| PMS2 | Plays a role in DNA repair and recombination |
| EPCAM | Involved in cell adhesion and signaling |
It’s key to know how hereditary nonpolyposis colorectal cancer syndrome works. This helps us find those at risk. With genetic testing, we can catch it early. Then, we can decide on prevention and checkup plans for Lynch syndrome cases.
Conclusion
Lynch syndrome is a hereditary condition that increases the chances of getting certain cancers. Genetic testing is key to find out who may have it and their cancer risk. This type of testing plays a big part in early detection.
Getting tested early and regular cancer screenings make a big difference. They can find cancer when it’s easier to treat. People with Lynch syndrome should always follow screening and check-up plans.
Genetic counseling is important for those with Lynch syndrome and their families. It gives them the facts, like their personal risk and what to do about it. Genetic counselors help people understand their options and make a plan for cancer protection.
Although researchers are looking into using stem cells to treat Lynch syndrome, it’s not ready yet. More studies are necessary to see if it’s safe and works well. While it might be a possible future treatment, stem cell therapy isn’t something widely done right now.
FAQ
Q: What is hereditary nonpolyposis colorectal cancer syndrome (HNPCC), also known as Lynch syndrome?
A: HNPCC is a cancer syndrome you get from your parents. It makes you more likely to get certain types of cancer. It happens when certain genes that repair DNA don’t work right.
Q: What cancers are associated with hereditary nonpolyposis colorectal cancer syndrome?
A: If you have HNPCC, you’re at a higher risk for many cancers. This includes colorectal, endometrial, gastric, and ovarian cancers.
Other risks are small bowel, pancreatic, and prostate cancers. You might also get urinary tract, bile duct, sarcoma, brain cancers, and skin tumors.
Q: How common is hereditary nonpolyposis colorectal cancer syndrome?
A: About 1 in 300 people have HNPCC. This makes it one of the more common cancer syndromes you get from your family.
Q: How is hereditary nonpolyposis colorectal cancer syndrome diagnosed?
A: Doctors diagnose Lynch syndrome using special criteria. They look at your family’s cancer history and your tumor’s DNA. If the DNA looks different, it could mean you have it.
Q: Can genetic testing help identify hereditary nonpolyposis colorectal cancer syndrome?
A: Yes, a genetic test can find if you have genes linked to Lynch syndrome. This test looks at the MLH1, MSH2, MSH6, PMS2, and EPCAM genes.
Q: How does hereditary nonpolyposis colorectal cancer syndrome inherit?
A: HNPCC is passed down from a parent in a special way. If a parent’s gene is changed and they have HNPCC, they might give it to their child.
Q: What is the role of genetic counseling in hereditary nonpolyposis colorectal cancer syndrome?
A: Genetic counseling is key for those with HNPCC. It informs about the condition. Plus, it aids in deciding on health choices wisely.
Q: Is stem cell therapy a potential treatment for hereditary nonpolyposis colorectal cancer syndrome?
A: Looking into stem cell therapy for HNPCC is interesting. Yet, we still need more studies to see if it really works.