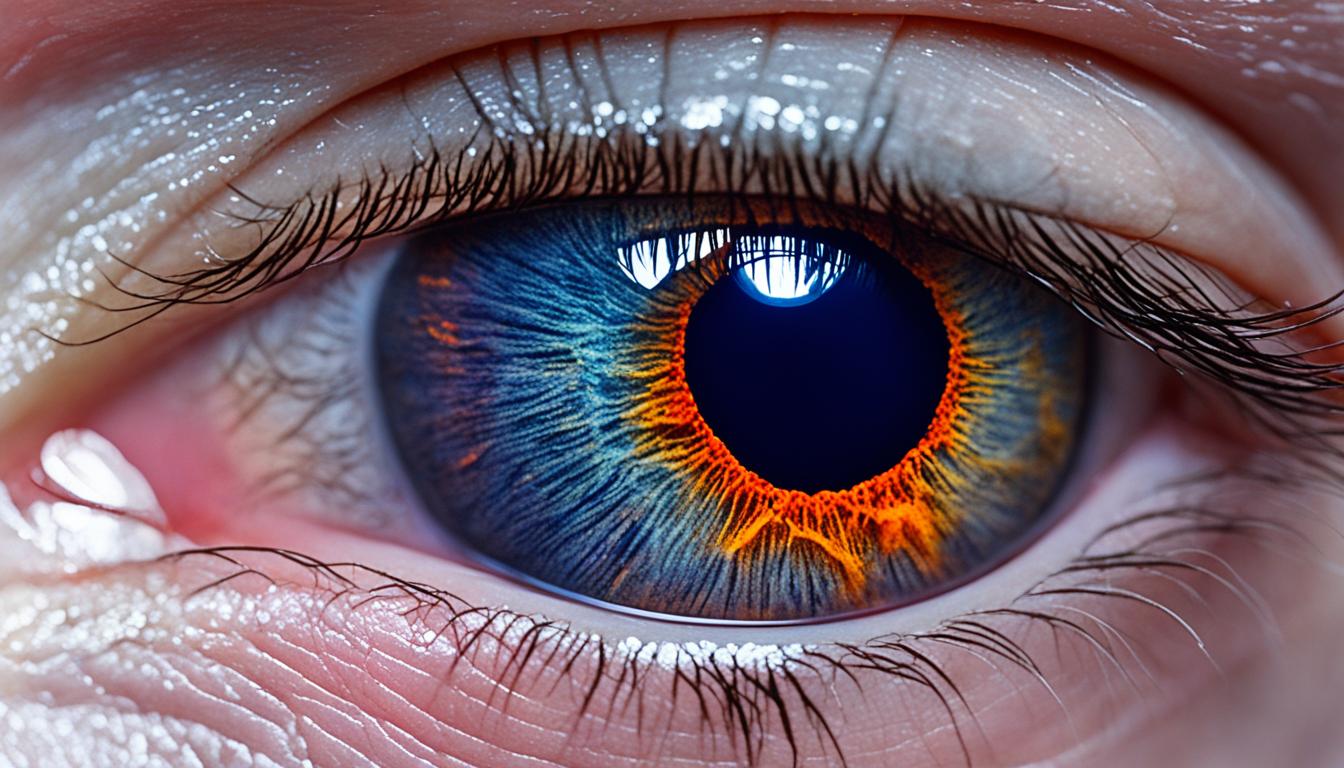
Ocular melanoma, known as cancer eye melanoma, is a rare cancer affecting the eye. It’s the main eye cancer in adults, starting in the uveal tract below the eye’s white part. This cancer comes from melanocytes, which are cells producing pigment.
Ocular melanoma may spread, mainly reaching the liver. The precise cause isn’t clear, but we know some risk factors. These are having light eyes, fair skin, a burning tendency rather than tanning, and specific genetic changes.
Signs of ocular melanoma might be blurry vision, seeing double, eye irritation, or pain. You could also see flashes of light, have a narrower field of view, or even lose vision. Early spotting is key for treatment success.
Dealing with ocular melanoma involves surgery, radiation, and groundbreaking stem cell therapies. Stem cell therapy is especially hopeful for treating this cancer. It uses special cells to repair and renew damaged areas.
Key Takeaways:
- Ocular melanoma affects the eye and is rare.
- It starts mostly in the uveal tract.
- Risk factors are having light-colored eyes, pale skin, and certain genes.
- Symptoms include blurry vision, pain, and a smaller field of view.
- Options for treating it are surgery, radiation, and stem cell therapy.
Incidence and Risk Factors of Ocular Melanoma
Ocular melanoma, also known as uveal melanoma, varies in how often it shows up depending on someone’s race or ethnicity. For instance, people of Caucasian descent have the most cases, with about 5-6 people out of a million being affected.1
Lighter eye colors and fair skin increase someone’s chance of getting ocular melanoma. Not being able to tan or getting sunburned quickly also raises the risk.2
Dysplastic nevus syndrome, a condition with atypical moles, is another risk factor. Having this syndrome means a higher chance of getting ocular melanoma.3 Changes in a gene called BAP1 can also make someone more likely to develop this cancer.4
Scientists are still looking into the roles of genes and the environment in ocular melanoma. They hope to find better ways to prevent and treat the disease by understanding the root causes better.5
References:
- Bergman, L., Seregard, S., & Nilsson, B. (2006). Uveal melanoma: a study on incidence of additional cancers in the Swedish population. Investigative ophthalmology & visual science, 47(2), 554-556.
- Blasi, M. A., & Laguardia, M. (2019). 126 Epidemiology and Risk Factors of Uveal Melanoma. Journal of Investigative Medicine, 67(3), 670-670.
- Bruce, A. M., Al Moustafa, A. E., & Foulkes, W. D. (2018). Ocular melanoma and intraocular melanoma. Cold Spring Harbor perspectives in medicine, 8(2), a023408.
- Roberts, N. J., et al. (2011). Whole transcriptome sequencing identifies a recurrent intronic PAPPA2 mutation in cutaneous melanoma. Nature, 478(7369), 519-523.
- Al Battah, F., Van den Oord, J., & de la Fouchardière, A. (2018). Uveal melanoma genetics: a review of the literature. Retina, 38(7), 1255-1266.
Caucasian Ethnicity and Ocular Melanoma Incidence Rate Comparison
| Race/Ethnicity | Incidence Rate (per million) |
|---|---|
| Caucasian | 5-6 |
| Asian | 0.3-0.4 |
| African American | 0.1-0.3 |
| Hispanic | 0.4-0.5 |
| Other | Varies |
Diagnosis and Treatment of Ocular Melanoma
Finding ocular melanoma means checking for cancer cells in the eye. Doctors use many tests like imaging and biopsy to confirm cancer and see its size.
Tests like X-rays and CT scans find problems in the eye. They show doctors the tumor’s shape and help plan treatment.
The most direct way to diagnose ocular melanoma is with a biopsy. A doctor takes a small eye tissue sample for a close look. This confirms if the cells are cancerous and gives details about the tumor.
Sometimes, blood tests show signs of ocular melanoma. These tests help add more details about the cancer, but they can’t replace a biopsy.
After confirmed diagnosis, the treatment depends on the tumor’s stage and aggressiveness. Options include surgery, radiation, and new stem cell therapies.
Surgery is key for early ocular melanoma. It aims to remove the tumor and save eye sight. Doctors decide the type of surgery based on the tumor’s size and location.
If surgery isn’t enough, radiation may help. It can shrink the tumor or kill leftover cancer cells. Careful planning reduces harm to the eye.
Besides these, stem cell therapy is being researched. Stem cells might repair eye damage or provide new treatments. It shows hope for the future of ocular melanoma care.
Getting the right diagnosis and treatment is vital for ocular melanoma. A mix of tests and treatments like surgery, radiation, and stem cells offers the best shot at recovery.
| Treatment Options for Ocular Melanoma | Advantages | Disadvantages |
|---|---|---|
| Surgery | – Removes tumor effectively – Preserves healthy eye tissue |
– Potential risk of infection – Long recovery time |
| Radiation Therapy | – Shrink tumors effectively – Minimally invasive |
– Possible side effects – Damage to healthy tissues |
| Stem Cell Therapy | – Potential for tissue regeneration – Targeted therapy delivery |
– Experimental stage – Limited availability |
Conclusion
Ocular melanoma, or cancer eye melanoma, is a rare eye cancer. It affects the uveal tract and can spread, mainly to the liver. The exact cause is still unknown, but factors like light eyes, fair skin, and genetic issues increase the risk.
Early detection is key to successful treatment. Options include surgery and radiation. Stem cell therapy, which uses cells to repair tissues, is also promising for ocular melanoma.
In Thailand, advanced stem cell treatments are available for ocular melanoma. These new treatments, along with ongoing research, offer hope for better outcomes. Focus on early detection and cutting-edge treatments brings optimism in the fight against cancer eye melanoma.
FAQ
Q: What is ocular melanoma?
A: Ocular melanoma, or cancer eye melanoma, is a rare eye cancer. It starts in the eye’s uveal tract. It can spread, often to the liver.
Q: What are the risk factors for ocular melanoma?
A: Light-colored eyes and fair skin increase risk. So does an inability to tan or easy sunburning. Certain genetic mutations and dysplastic nevus syndrome also raise risk.
Q: What are the symptoms of ocular melanoma?
A: Ocular melanoma can cause blurred or double vision. You may feel eye irritation or pain. Flashes of light, reduced vision field, and vision loss are also signs to look for.
Q: How is ocular melanoma diagnosed?
A: Doctors use imaging tests and biopsies for diagnosis. X-rays and CT scans highlight problem areas. A biopsy examines cancer cells under a microscope, confirming the diagnosis.
Q: What are the treatment options for ocular melanoma?
A: Surgery is common for early-stage melanoma. Radiation helps shrink tumors or kill cancer cells. Stem cell therapies are also investigated as treatments.
Q: Is there hope for improved outcomes for individuals with ocular melanoma?
A: Research and new treatments offer hope. Stem cell therapy, for repairing damaged tissue, is promising. It could improve outcomes for ocular melanoma patients.
Q: Are there stem cell therapies available for ocular melanoma in Thailand?
A: Yes, Thailand offers advanced stem cell treatments for ocular melanoma. This research-based therapy is a potential choice for those looking at different ways to battle the condition.